Given the profound disruption that multiple sclerosis (MS) can cause in patients’ lives, researchers are eager to try to find ways in which it can be predicted earlier and monitored more precisely. One group of investigators decided to retrospectively analyze ophthalmological, neurological, radiological and laboratory data in MS patients to look for any potential biomarkers.
Structural OCT was used to look at the retinal nerve fiber layer (RNFL) and ganglion cell complex (GCC), while OCT angiography (OCT-A) assessment of vascular density (VD) was performed. Best-corrected visual acuity and ophthalmological biomicroscopy of the anterior segment and fundus were also evaluated.
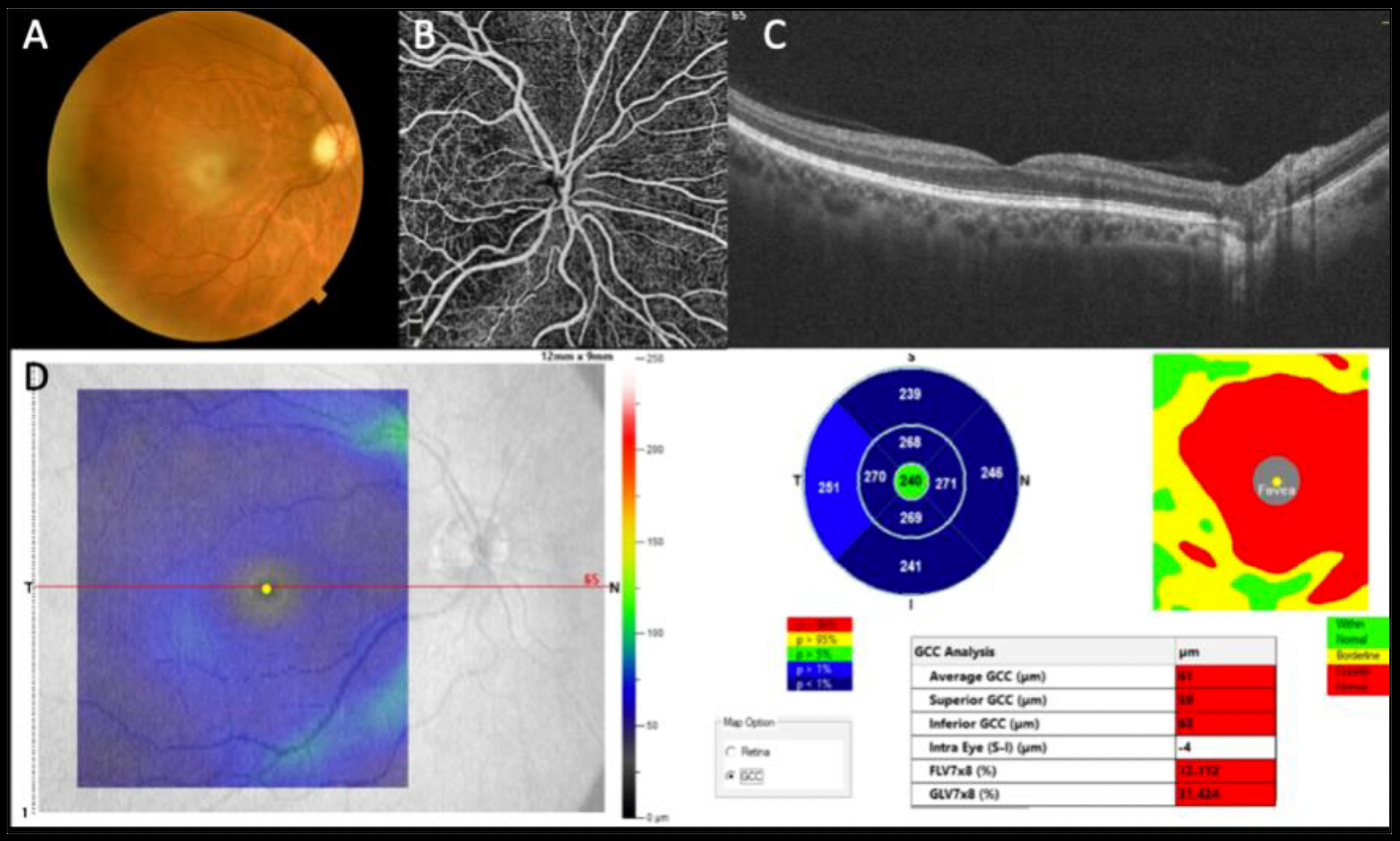 |
| This image from the study shows a normal optic nerve in Fig. (A), wherein the posterior pole and midperiphery shows no severe morphologic changes. However, in Fig. (B) OCT-A reveals a reduction in the deep vascular pattern most evident at the posterior pole and particularly at the interpapillary-macular bundle, and the OCT B-scan in Fig. (C) reveals a reduction in the inner retinal layers where nerve fiber layers are located. In Fig. (D), we see an average reduction in the ganglion cell layer at the posterior pole compared with normative data (blue color map). Photo: Savastano MC, et al. Am J Ophthalmol. June 18, 2024. Click image to enlarge. |
Of the 106 patients (212 eyes) included, 62.2% had MS and 37.8% (40 eyes) were matched healthy controls. Those with MS displayed lower RNFL, GCC and VD in the radial peripapillary capillary plexus than controls in both eyes. Using logistic regression of distinct MS outcomes for both eyes, the value most predictive of MS was the average GCC thickness. More analysis uncovered that a higher T2-weighted lesion showed lower RNFL thickness value and reduced GCC and VD values than those with a low lesion load. Relapsing MS patients also displayed lower RNFL values.
The authors relay the importance of their findings, stating that, “to date, despite technological advancements, there are few prognostic biomarkers of the MS disease course and disability that re not easily applicable in clinical practice.” One advantage of OCT is that it is a non-invasive imaging technique and also provides high-resolution quantification of retinal structures such as the ones measured in this study.
The study authors analyzed RNFL, GCC and VD in the peripapillary area of 66 patients with and without optic neuritis history due to MS, finding similar significant reduction in these values as previous studies when compared with the control group.
This group of researchers also found a significant decrease in peripapillary VD in eight eyes with and 124 eyes without history of optic neuritis compared with the control group. This reflects previous studies finding a marked decrease in optic nerve head circulation in MS patients without optic neuritis history.
They also point out that the significant association seen between disability status at diagnosis and at ophthalmological control and peripapillary VD values—specifically in the left eye—may be due to 40% of evaluated patients experiencing retrobulbar optic neuritis at the outset, with 66% of those cases showing left eye involvement.
Because a higher T2-lesion load upon MRI correlated with reduced average RNFL, GCC and peripapillary VD values, and that average RNFL thickness values corresponded with disease reactivation, the authors believe that “our data support the importance of OCT and OCT-A as minimally invasive, rapid and non-operator-dependent examinations to provide crucial data regarding the potential clinical course of MS.”
Savastano MC, Nociti V, Giannuzzi F, et al. Optical coherence tomography advanced parameters in patients with multiple sclerosis: ophthalmological and neurological assessments. Am J Ophthalmol. June 18, 2024. [Epub ahead of print]. |


