 |
|
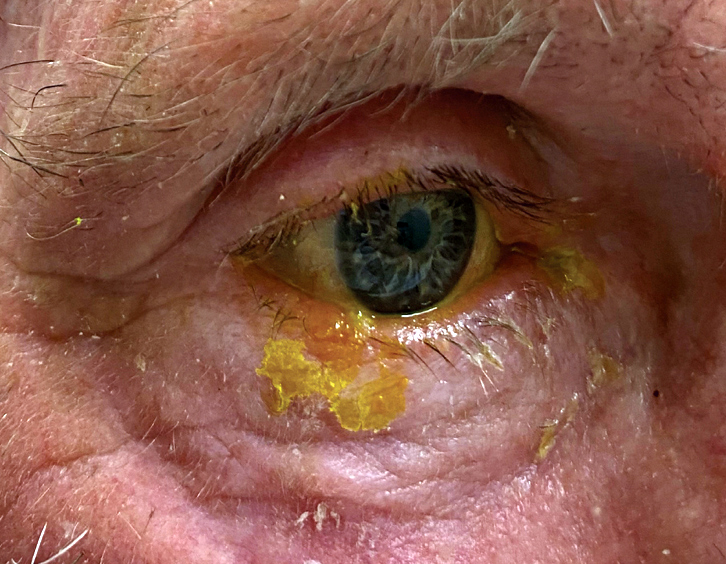
HZO may be triggered by cataract surgery, as recurrence occurred in 40% following surgery, as well as increased recurrence being associated with shorter quiescence periods and those who have a greater number of recurrences before surgery. Photo: Joseph W. Sowka, OD. Click image to enlarge. |
In the largest report to date, one group of researchers investigated the long-term outcomes of patients with herpes zoster ophthalmicus (HZO). They focused on looking at recurrence frequency, risk factors and long-term clinical outcomes. Their paper on the work was published in American Journal of Ophthalmology last Friday.
The retrospective study included 869 patients with acute HZO who were seen at a single care center from 2006 to 2016; median follow-up time was 6.3 years (range 3.7 to 8.9 years). The primary outcomes measure was recurrence of the disease, with a secondary outcome measure of rate of moderate vision loss (≤20/50).
A total of 551 recurrences were observed, with at least one recurrence happening in 23% (n=200) of cases, with uveitis being most common at 34.8%. Median time to first recurrence incidence was 3.5 months, with predictors of recurrence being immunosuppression, higher presenting intraocular pressure, corneal involvement and uveitis. In the first month of presentation, topical steroids were given in 437 cases, with recurrence in this group reaching 42.1% (n=184). After cessation of topical steroid treatment, recurrence happened at a median of 1.4 months but became 90% within seven months. Moderate vision loss was seen in 15.5% of patients with zero recurrences, 28.6% with one, 31.4% with two, 50.0% with three and 57.4% with four or more.
In their discussion, the authors note that age and presenting vision were significant factors predicting recurrence on univariate analysis but were not significant upon multivariate analysis. They also add that prior investigations on this topic have used shorter follow-up periods and report a high recurrence rate within the first couple years after rash onset. However, the authors do report that their 3.5-month recurrence rate is similar to previous studies.
They continue that their results did not show initiation of topical steroids or frequency of treatment at disease onset to be significantly associated with recurrence risk. Delayed steroid onset did display lower disease recurrence risk, perhaps reflecting lower disease severity in those with delayed steroid onset or the impact of steroids on viral virulence and future risk of recurrence. This, along with the inverse of steroid cessation being predictive of relapse risk, “highlights the importance of close monitoring with a careful tapering regimen. The ideal follow-up regimen for HZO needs to be personalized and in the context of ophthalmic issues, both active and inactive.”
The investigators also highlight that recurrence rate and severity of HZ are much higher for immunosuppressed patients, with less than 2% of individuals with HZ being immunocompromised but who are 51% more likely to develop HZ with a 25% higher risk of recurrence. The rate in this study of immunocompromised patients was 9.5%, either by systemic disease or immunosuppressive therapy, with the most common immunosuppressive drugs being corticosteroids, disease-modifying antirheumatic drugs and chemotherapy.
Importantly, the authors suggest that “the high rate of immunosuppression and recurrence identified in our study highlights the importance of identifying these patients and considering a longer course of treatment with closer monitoring for disease recurrence.”
Not just recommended for immunosuppressed patients, though, the authors more generally state that “these findings indicate the need for close monitoring for potential recurrences, especially after cessation of topical steroid treatment and in those with identified risk factors for recurrence.”
Scott DAR, Liu K, Danesh-Meyer HV, Niederer RL. Herpes zoster ophthalmicus (HZO) recurrence: risk factors and long-term clinical outcomes. Am J Ophthalmol. June 21, 2024. [Epub ahead of print]. |


