 |
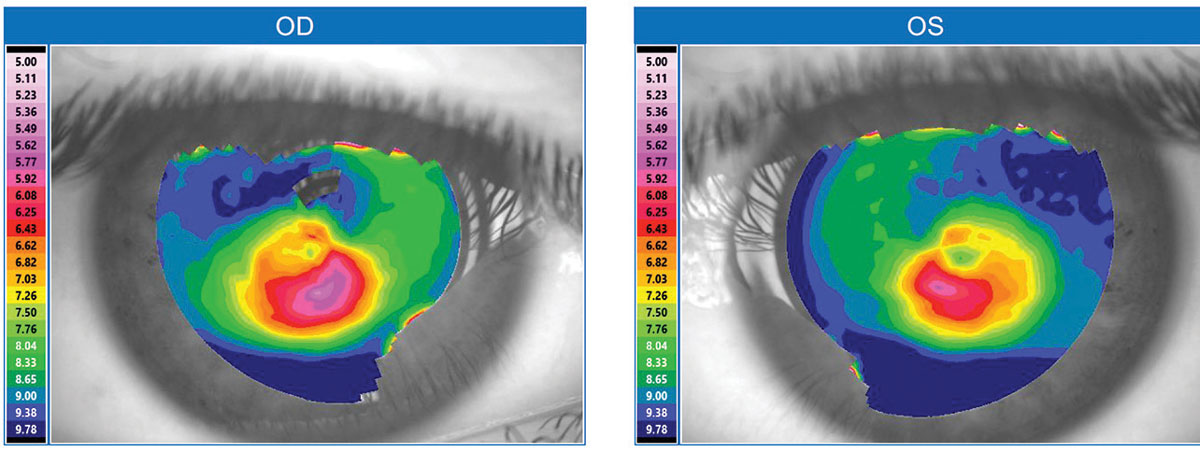
| Evaluating corneal topography may help predict keratometric changes in patients who may be required to suspend GP lens use. Photo: Brian Chou, OD. Click image to enlarge. |
Detecting keratoconus progression helps determine when corneal crosslinking (CXL) is most opportune, but rigid gas permeable (GP) lens use by these patients can alter certain corneal metrics and thus may confound the assessment of patients for CXL candidacy. Researchers recently found that keratometry and spherical components of the anterior corneal surface decreased in GP lens wearers, with greater changes observed in eyes with more severe disease. Corneal progression indices, including corneal thickness, posterior keratometry and irregular astigmatism values, mostly remained unchanged.
The study included 31 eyes of 31 patients diagnosed with keratoconus. The patients hadn’t used GP or any other type of contact lens for at least one month. Corneal topographic data was obtained using 3D anterior segment OCT before and after one month of GP lens use.
The average and maximum keratometry values changed with GP lens wear (-1.05D and -1.65D, respectively), and the spherical component of the anterior corneal surface became significantly smaller. No change was observed in the central or thinnest corneal thickness values. Keratometric changes were greater in eyes with severe keratoconus than in those with moderate keratoconus.
“It is important to consider these findings when evaluating corneal topography of keratoconus and preparing CXL,” the study authors concluded in their paper. “It may help predict keratometric changes in patients who may be required to suspend GP lens use.”
Akiyama K, Ono T, Ishii H, et al. Impact of rigid gas-permeable contact lens on keratometric indices and corneal thickness of keratoconus eyes examined with anterior segment optical coherence tomography. PLoS One. July 8, 2022. [Epub ahead of print]. |


