In a two-year real-world prospective study, researchers from Milan attempted to discover which clinical and imaging biomarkers were associated with the onset of outer retinal atrophy in patients with age related-macular degeneration (AMD).
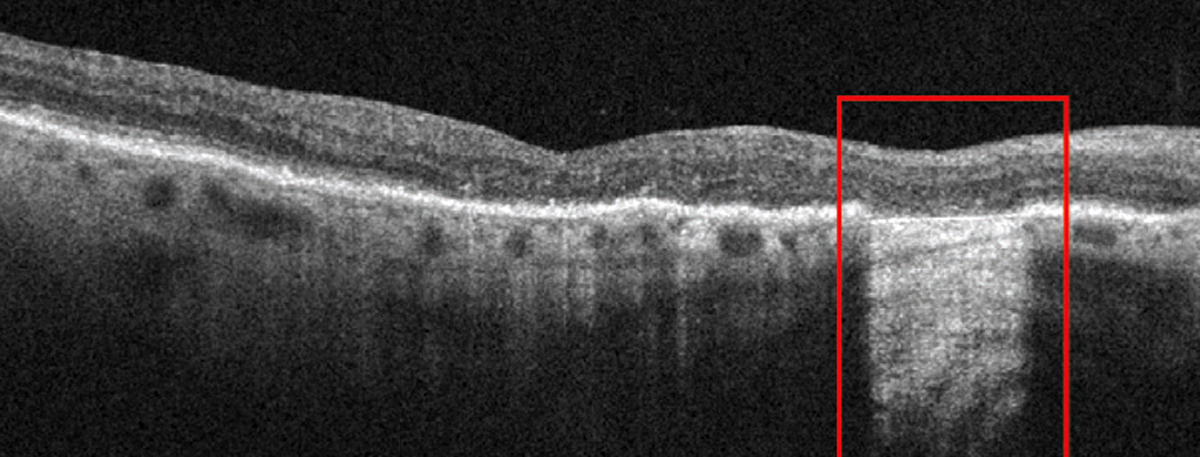 |
| Outer retinal atrophy in a dry AMD patient not part of this study. Photo: Anna Bedwell, OD. Click image to enlarge. |
This study’s cohort consisted of 370 eyes from 370 AMD patients treated with anti-VEGF intravitreal injections. Additionally, 84 eyes (23%) switched anti-VEGF treatments during the two-year follow-up period. Before the study began, six eyes (2%) presented with complete outer retinal atrophy. After two years, a total of 120 eyes (33%) were observed to have complete outer retinal atrophy during their follow-up visit.
In order to identify which biomarkers were linked to onset outer retinal atrophy, the researchers collected noninvasive imaging metrics using OCT, OCT angiography (OCT-A) and fundus autofluorescence. The researchers noted in their study that only 145 eyes were analyzed using OCT-A; the remaining data was discarded due to subpar scan quality or artifacts.
Macular neovascularization was also observed and classified in the study’s results. A total of 198 eyes (54%) were classified as Type 1, 89 eyes (24%) were classified as Type 2, 29 eyes (7%) were classified as polypoidal choroidal vasculopathy, and 54 eyes (15%) were classified as Type 3. Researchers reported that polypoidal choroidal vasculopathy and Type 3 classifications were associated with a higher risk of outer retinal atrophy.
“We confirmed that Type 3 and aneurysmal Type 1 macular neovascularization were associated with worse visual outcomes and higher onset of complete outer retinal atrophy,” reported the researchers in their study. “Conversely, Type 1 and Type 2 macular neovascularization lesions were well managed by anti-VEGF injections.”
There were a number of biomarkers that were associated with the onset of outer retinal atrophy. The researchers discovered that the presence of intraretinal fluid, thinning of the Sattler choroidal layer, switching to different anti-VEGF agents late in treatment, a lower number of anti-VEGF injections and the perfusion characteristics of the macular neovascularization were all relevant biomarkers. Other biomarkers showed lower significant values and therefore were not relevant factors associated with onset of outer retinal atrophy.
Since much of the OCT-A data was discarded, this limited the results of the study. Furthermore, the researchers believed that the two-year follow-up period did not warrant enough time to elicit a sufficient number of significant results in their study. They also believed that a good portion of participants in their study received a proper number of intravitreal injections, which led to less significant results. They propose that further studies will need to assess the course of macular neovascularization and the effect of both optical coherence tomography and optical coherence tomography angiography parameters on different stages of outer retinal atrophy in greater detail. “Future studies should be focused on the development of customized anti-VEGF treatment strategies, based on quantitative multimodal imaging, to optimize treatment effects and to improve clinical outcomes,” concluded the researchers in their study.
Arrigo A, Saladino A, Aragona E, et al. Clinical and imaging biomarkers associated with outer retinal atrophy onset in exudative age-related macular degeneration: A real-word prospective study. Ophthalmol Ther. March 6, 2024. [Epub ahead of print]. |


