 |
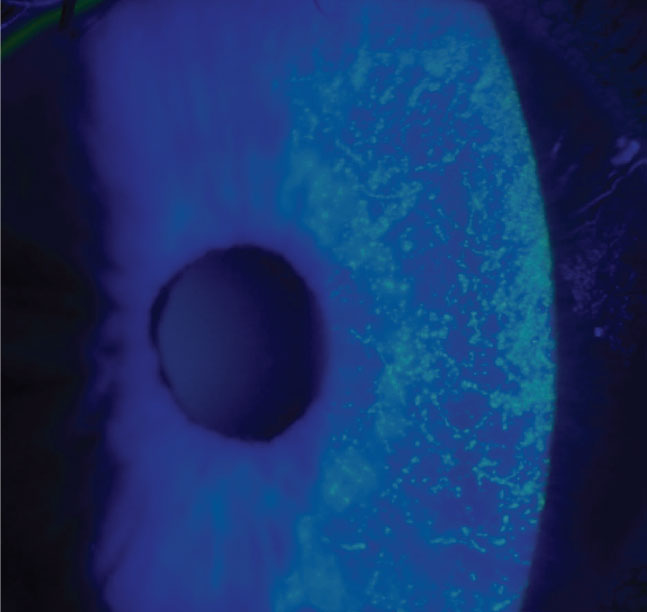
Results from this study demonstrated a correlation between dry eye and HOAs. Photo: Katherine Sanford, OD. Click image to enlarge. |
Patients with higher-order aberrations (HOAs) may see distorted or blurry images that cannot be corrected with glasses or contact lenses. A critical component of the pathophysiology of this condition is the tear film, which after undergoing a change in thickness, may introduce aberrations and cause functional irregularity of this important, hydrating structure. Dry eye has already been proven in many studies to increase the risk of HOAs through the disruption of the tear film. So, does this mean that improving dry eye severity could reduce the incidence of HOAs?
To answer this question, a research group searched through articles in the Entrez PubMed database that included the phrases ‘‘higher-order aberrations and dry eyes.” After excluding irrelevant entries, the group ended up with 27 unique papers on the topic, 12 of which observed associations between dry eyes, HOAs and HOA parameters and 15 of which looked at dry eye interventions and HOA outcomes and parameters.
Of the 12 papers on dry eye and HOA outcomes, eight found an existing correlation. Observations across the other four differed, though several studies did identify an association between tear breakup time (TBUT) and HOA amount. “In one paper, although the differences in HOAs between normal and dry eyes were not assessed, TBUT was significantly less in dry eyes compared with normal eyes and total HOAs were decreased after saline drops in both patients with normal and dry eyes,” the researchers wrote in their paper.
“The last two case reports by the same group showed an opposite phenomenon where HOAs were increased after blinking in post-punctal plug placement patients and in patients with short TBUT,” they continued. “HOAs tend to increase in normal patients and patients with dry eye post-blink due to disruption and changes in the tear film. Before the tear film breaks up, the difference in tear film thickness of the thinner superior and thicker inferior cornea may lead to delayed wavefronts inferiorly and increased coma-like aberrations. Similarly, punctal occlusion in some cases of mild dry eye may cause visual impairment due to the post-blink movement of excessive tear volume.”
As for the 15 papers which looked at dry eye interventions and HOA outcomes, 12 reported some level of improvement in HOAs after eye drop therapy. The type of drop used and its viscosity as well as dry eye disease (DED) severity all seemed to have a significant impact on aberrations. “The turnover of tear film components, in particular the lipid components, plays an important role in the effectiveness of eye drops and is an important aspect to consider when utilizing lipid-based eye drop treatments,” the researchers explained.
“Overall, there is evidence to show that an association between dry eyes and HOAs exists and that treating DED through interventions including eye drops, secretagogues and punctal plugs can improve HOA outcomes,” the group concluded. The effectiveness of these interventions in limiting HOAs still needs to be explored in future studies for the sake of this rapidly growing DED patient population and the clinicians who provide them with care.
Rhee J, Chan TCY, Chow SSW, et al. A systematic review on the association between tear film metrics and higher order aberrations in dry eye disease and treatment. Ophthalmol Ther. November 11, 2021. [Epub ahead of print]. |


