 |
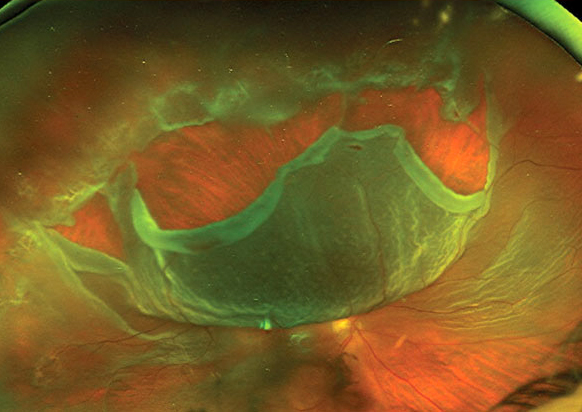
| Patients who weren't vaccinated at time of retinal detachment diagnosis had worse clinical outcomes in this study cohort. Photo: Mohammad Rafieetary, OD. Click image to enlarge. |
A recent study sought to determine how reluctance to getting the COVID-19 vaccine could affect clinical trends and presentation of primary rhegmatogenous retinal detachment (RRD), an urgent condition typically requiring immediate surgery. The World Health Organization defines vaccine hesitancy as a delay or refusal of immunization. According to the single-center data of this recent study, those who were vaccinated at presentation or within a year after had significantly better initial and final best-corrected visual acuity (BCVA) than those who remained unvaccinated.
The research group performed a retrospective cohort study on 1,047 patients diagnosed with RRD between December 2020 and December 2021. For purposes of this study, being vaccinated was defined as having received at least one dose of the Pfizer or Moderna vaccine or the single-dose Johnson & Johnson vaccine. Patients were divided into three groups according to vaccine status or hesitancy: presenting vaccinated (Prior-Vax; n=391), subsequently getting vaccinated (Later-Vax; n=252) or remaining unvaccinated (Never-Vax; n=404).
Significantly more patients in the Never-Vax and Later-Vax cohorts presented with macula-off RRDs compared with the Prior-Vax cohort (57.9% and 54% vs. 44.5%, respectively). Primary proliferative vitreoretinopathy was also more common in the Never-Vax and Later-Vax groups than in the Prior-Vax group (17.1% and 13.6% vs. 4.3%, respectively).
Compared with the Never-Vax group, both the Prior-Vax and Later-Vax groups had lower rates of either pars plana vitrectomy (PPV) alone or combined scleral buckle and PPV, and higher rates of complex retinal detachment repair, although no significant differences were observed in rates of other included procedures (pneumatic retinopexy, primary scleral buckle and primary PPV).
Significantly more patients were lost to follow-up in the Never-Vax group compared with the other two groups (7.7% vs. 2.2%, respectively), and unvaccinated patients also had to travel further on average than the Prior-Vax and Later-Vax cohorts (median of 35 miles vs. 22.3 miles, respectively). See the table below for a breakdown of each group’s initial and final BCVA.
Based on these findings, the researchers concluded in their paper on the work, “COVID-19 vaccine hesitancy is associated with worse clinical presentation and outcomes for primary RRD.” They suggested taking this data into consideration when treating vaccine-hesitant patients.
Table 1. Vaccine Status and BCVAs in RRD Patients
Initial logMAR BCVA | Final logMAR BCVA | |
Prior-Vax | 0.30 | 0.18 |
Later-Vax | 0.54 | 0.30 |
Never-Vax | 0.70 | 0.40 |
Mundae R, Wagley S, Ryan EH, et al. COVID-19 vaccination hesitancy and its association with altered presentation of primary rhegmatogenous retinal detachment. Am J Ophthalmol. May 13, 2022. [Epub ahead of print]. |


