 |
|
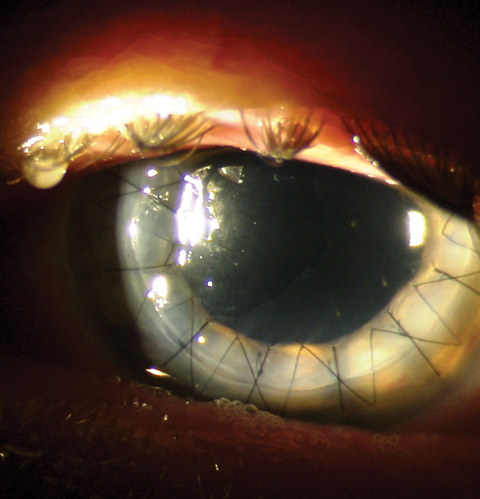
Though still a rare occurrence, corneal ulcers brought on through contact lens wear led to penetrating keratoplasty more often than those arising from refractive surgery. Image courtesy of Mitch Ibach, OD. Click image to enlarge. |
Newer technology has improved the safety profiles of contact lenses (CLs) and LASIK, but risks and complications still remain, such as corneal abrasions, infectious corneal ulcers and acquired limbal stem cell deficiency. Most can be addressed with phototherapeutic keratectomy for scarring or crosslinking for ectasia, but sometimes a penetrating keratoplasty (PK) is necessary. Noting a gap in the literature comparing CL and LASIK outcomes leading to severe complications requiring PK, researchers recently performed a cross-sectional analysis spanning 10 years to compare incidences and outcomes in this population. They found that patients undergoing PK secondary to CL use trended higher than LASIK.
The retrospective chart review included all patients who underwent keratoplasty in a specific US metropolitan area. The main outcome measure was BCVA at two years, and the secondary outcome measure was the relative risk of undergoing PK secondary to a CL or LASIK complication.
The analysis included 46,545 CL users and 10,285 patients who underwent LASIK during the study period. A total of 24 CL users (0.52 per 1,000) and three post-LASIK patients (0.29 per 1,000) underwent PK secondary to complications. In the CL cohort, BCVA at two years was 1.45 logMAR (20/564 Snellen), and in the post-LASIK cohort, BCVA was 0.07 logMAR (20/23 Snellen) following PK.
“The incidence of complications leading to PK in CL users and post-LASIK patients was found to be low in our overall study population and not statistically different between groups, although there was a trend toward a higher frequency in CL wearers,” the researchers noted in their study. “However, patients undergoing PK secondary to CL-associated complications had significantly worse visual outcomes at two years compared with those with LASIK-associated complications.”
“An alarming number of patients, 40% and 12%, who underwent PK secondary to a CL-associated complication ended up legally blind and with no light perception, respectively,” they pointed out. “These findings suggest that patient perceptions regarding implied or absolute safety of CL may be misplaced. This study helps underscore the fact that, relative to routine CL wear, refractive surgery is a safe alternative and does not increase the risk for substantial vision loss due to a complication.”
The researchers concluded that further research to evaluate these findings and determine more factors to improve safety and mitigate risk are needed for all forms of refractive correction beyond glasses.
Rush SW, Bulla B, Rush RB. Complications leading to keratoplasty among contact lens users and LASIK patients: a 10-year cross-sectional analysis. J Ophthalmol. August 14, 2021. [Epub ahead of print]. |


