 |
|
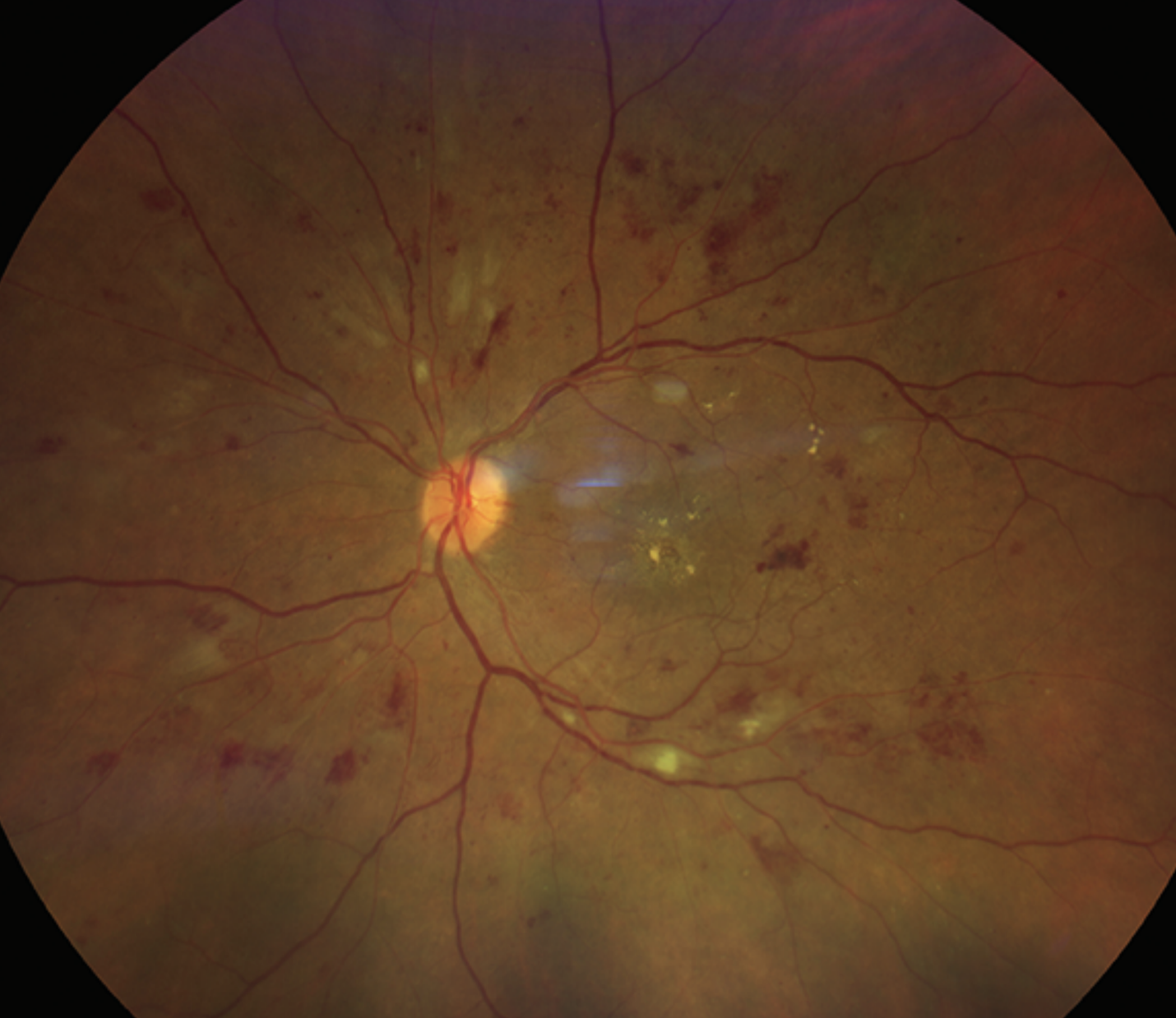
An inverse association was observed in this study between elevated levels of dyslipidemia markers and the risk of receiving a DR diagnosis. Photo: Rami Aboumourad, OD. Click image to enlarge. |
Current literature describes lipid abnormalities as a potential risk factor for the development and progression of diabetic retinopathy (DR). Interestingly, a new study found that reduced or elevated levels of certain lipid markers might help some patients stave off the condition. Its researchers observed an inverse association between elevated markers of dyslipidemia and the risk of receiving a DR diagnosis, though after diagnosis, the association disappeared.
The researchers evaluated electronic medical records of adults with type 2 diabetes in a United States national database, identifying 1,126,231 eligible patients (mean age: 60.8). The cohort was divided into groups based on the presence of abnormal serum levels of various lipid markers, including LDL, high-density lipoproteins (HDL), total cholesterol, triglycerides, Lp(a), apolipoprotein A-I (ApoA-I), apolipoprotein B (ApoB) and ApoB/ApoA-I ratios.
In patients without prior DR, the following lipid markers were associated with a decreased risk of receiving a DR diagnosis: low HDL (hazard ratio=0.94), total cholesterol (HR=0.88) and high triglyceride (HR=0.91). For patients with preexisting DR, the researchers found that having high LDL levels was associated with an increased risk of diabetic macular edema (HR=1.42), while having low HDL levels was associated with a slightly decreased risk (HR=0.92).
“The results of the present study suggest that, among patients with type 2 diabetes mellitus, reduced levels of HDL and elevated levels of total cholesterol and triglycerides may play a protective role against the development of DR, while reduced HDL levels and elevated LDL levels are associated with an adverse prognosis of DR,” the researchers summarized in their paper, published recently in Eye.
Given that dyslipidemia is a risk factor for other retinal diseases, it may seem counterintuitive that this study associated these lipid abnormalities with a reduced risk of DR diagnosis, the authors pointed out. They offered a potential explanation in their paper: “Although DR is characterized by altered vascular homeostasis, this alteration may predominantly be driven by mechanisms that are distinct from other vascular pathologies. This hypothesis is further supported by the fact that, whereas elevated Lp(a) levels and ApoB/ApoA-I ratio are known predictors of cardiovascular events, our study did not find a difference in the rates of DR development between patients who had normal and abnormal Lp(a) levels or apolipoprotein profiles.
“Another intriguing aspect of our results is that the observed negative associations between markers of dyslipidemia and the risk of DR development may appear to challenge the findings from previous studies that demonstrated the therapeutic potential of lipid-lowering agents—particularly, statins and fibrates—in preventing DR,” the authors continued. While this topic warrants further study, they note, two large, randomized control trials have presented evidence that fibrate therapy can significantly reduce DR risk. “As first-line pharmacological treatment of hypertriglyceridemia, fibrates significantly reduce circulating triglycerides levels and cause a modest reduction in total cholesterol levels and increase in HDL levels,” they wrote.
In conclusion, the authors pointed out that while dyslipidemia is known to increase the risk of DR, “this may be a nuanced relationship that is influenced by several factors, such as individual variances in the predominating pathological mechanisms and lipoprotein subfraction profiles.” In the future, they suggest, “delineating specific patient characteristics that may modulate the impact of various lipid markers on the development and progression of DR could provide particularly valuable insights into how clinicians should tailor their approach to screening or counselling diabetic patients based on their individual characteristics.”
Jeong H, Maatok CM, Russell MW, Singh RP. Associations between lipid abnormalities and diabetic retinopathy across a large United States national database. Eye. March 23, 2024. [Epub ahead of print]. |


