 |
|
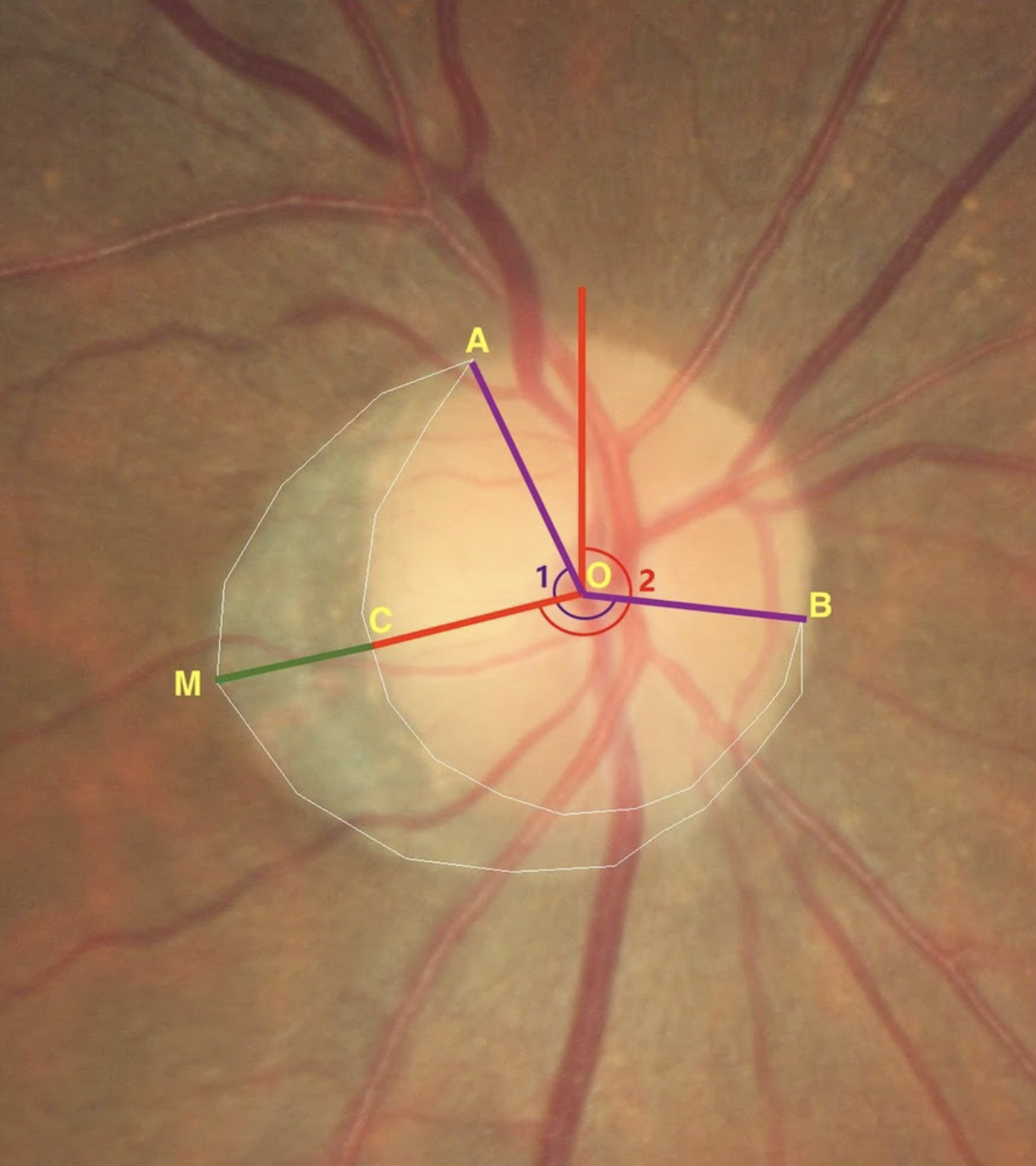
In a retrospective cohort study conducted in South Korea, researchers found longer radial extent and larger angular extent of beta-zone parapapillary atrophy were significantly associated in progression, suggesting this could be a predictive tool used in clinical practice. In this image (from a different study), point O is the center of the disc, and point A and B is the vertices of the beta zone, the point M and C is the maximum radial extent on the beta zone margin and disc margin. The beta zone is the area inside the white line, circumferential angle of the beta zone was defined as the angle between point A and B (angle 1), location of the beta zone was defined as the angle between maximum radial extent and vertical line from the center point of disc (angle 2), distance from C to M was defined as maximum radial extent of the beta zone. Photo: Zhou LX, et al. BMC Ophthalmol. 2022; 22:431. Click image to enlarge. |
Identifying factors that influence glaucoma progression has become increasingly important to researchers and, with each study published, physicians are better prepared to manage their patients’ disease. For instance, a body of research supports the role of parapapillary atrophy (PPA) on glaucoma progression, including the specific connection between beta-zone PPA and progression. A new study published in American Journal of Ophthalmology connects baseline beta-zone PPA morphology with progression in patients with primary open-angle glaucoma (POAG) using optical coherence tomography (OCT) guided progression analysis (GPA).
Researchers found that longer radial extent and larger angular extent of beta-zone PPA were significantly associated with progression on OCT GPA, as was the presence of disc hemorrhage. The study included 210 patients with POAG who had visited the Seoul National University Hospital in Korea between 2010 and 2020 and who were followed for a minimum of five years. Each participant had a clearly detectable beta-zone PPA at baseline and underwent retinal nerve fiber layer (RNFL) and optic nerve head (ONH) imaging via OCT annually. Presence of beta-zone PPA was defined as a chorioretinal-atrophied area with visible sclera and optic-disc-adjacent choroidal vessels.
Furthermore, the study classified beta-zone morphology into “crescent-type” and “solar-eclipse type” based on the 180-degree angular extent, as well as on the radial extent value, which is an average value of the population. If the radial extent was shorter than the average, PPA morphology was classified into “Type 1” and “Type 2” if longer. Rapid progression was identified in this order: Solar-eclipse type 2, Crescent type 2, Solar-eclipse type 1, Crescent type 1.
“The significant differences in glaucoma progression and RNFL change rate among these beta-zone PPA types further emphasize the clinical relevance of PPA morphology,” wrote the researchers in their paper. “Our results suggest that the frequency and rate of glaucoma progression will be higher and faster in beta-zone PPA types with larger radial and angular extents. Furthermore, in the comparison between crescent type 2 (PPA with only longer radial extent) and solar-eclipse type 1 (PPA with only larger angular extent), it is anticipated that Crescent type 2 will lead to a faster and more frequent progression of glaucoma. Although the exact mechanisms underlying these findings remain unclear, beta-zone PPA area likely reflects the vascular and mechanical vulnerability of the area surrounding the ONH.”
Among the limitations acknowledged by the authors, the first was the potential selection biases due to participant recruitment from one hospital who were exclusively of Korean ethnicity. “Replication of the study in diverse populations would enhance the external validity of the results,” they said. “[Also], we analyzed glaucoma progression only by changes in RNFL thickness. There are structural and functional test methods using various equipment to evaluate glaucoma progression, but it is difficult to achieve uniformity in the evaluation of progression if multiple test methods are included. For this reason, RNFL thickness change was chosen as the representative method, as the RNFL is not only in close proximity to the ONH but also provides a comprehensive measure of structural changes associated with glaucoma progression.”
The authors concluded that their study highlights the crucial role of beta-zone PPA morphology in prediction progression in POAG patients. They further state that their classification system is a useful framework for characterizing PPA morphology. “These classifications enable clinicians to stratify glaucoma patients into risk groups, thereby facilitating more targeted and personalized treatment strategies,” they wrote. “Decision tree analysis as demonstrated herein further simplifies risk assessment by identifying disc hemorrhage and PPA type as the primary determinants of progression on GPA. This approach, allowing for early intervention in the cases of patients at higher risk of glaucoma progression, has crucial practical implications for clinical practice. Further research and validation studies may refine the use of PPA morphology as a predictive tool in clinical practice, ultimately improving early detection and management of glaucoma.”
Huh MG, Jeong Y, Shin YI, Park KH, Jeoung JW. Can baseline parapapillary atrophy morphology predict future glaucoma progression?: An OCT glaucoma imaging study. American Journal of Ophthalmology. May 30, 2024. [Epub ahead of print.] |


