 |
|
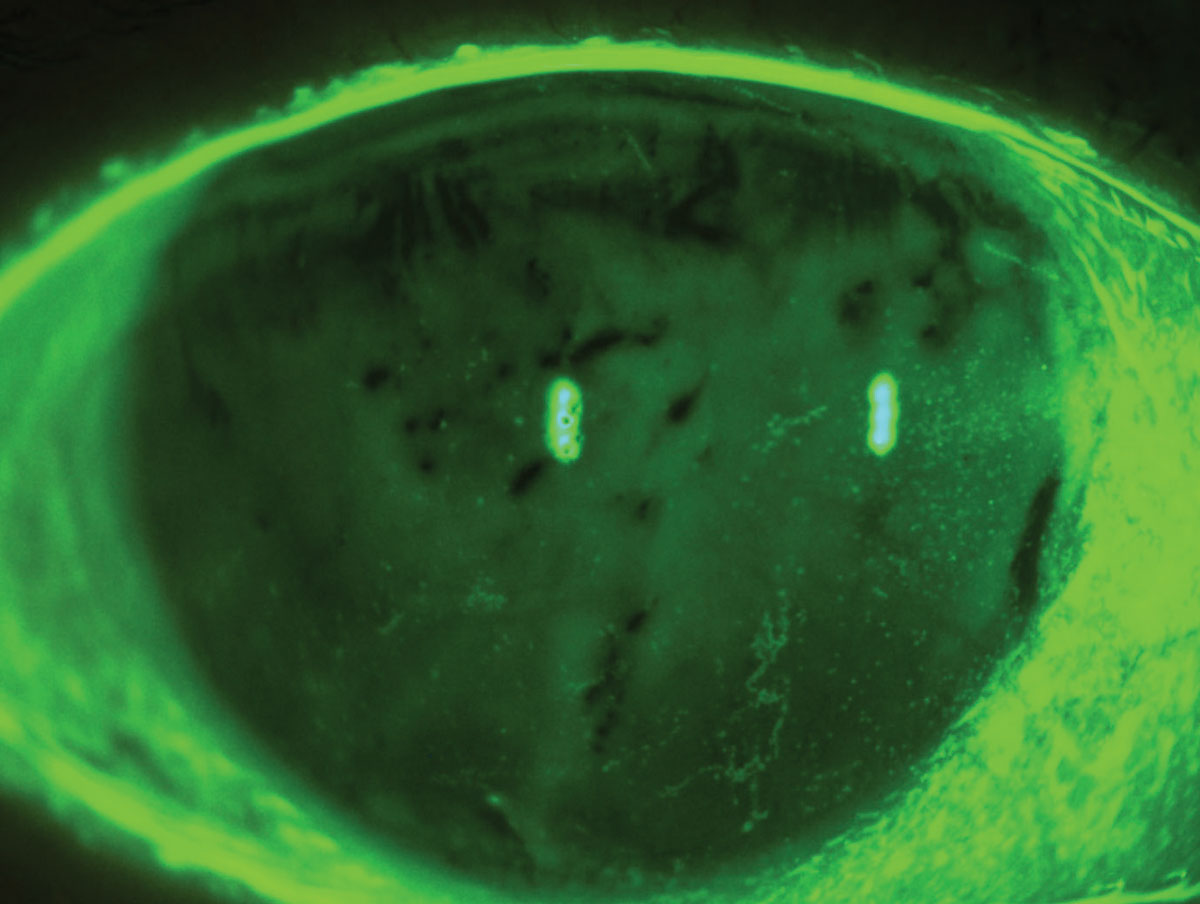
Hyabak was the only drop categorized as hypo-osmolar compared to human tears (osmolarity less than 275 mOsm/L). Other drops are categorized as iso-osmolar (osmolarity similar to human tears). Photo: Luis Rojas, OD. Click image to enlarge. |
Dry eye disease cases have greatly increased due to modern digital screen habits, environmental changes, polypharmacy and extended life expectancies.1 Although there are various prescription drugs for dry eye disease management, patients often self-medicate with other-the-counter artificial tears. In an attempt to understand the immediate impact of such eye drops on dry eyes, a team of Columbian researchers turned to 2017’s Dry Eye Workshop II (DEWS II) for inspiration on how to better understand the disease and develop a new study.
The basis for this study is rooted in the framework presented in DEWS II, which explained that dry eye is a multifactorial disease and noted that hyperosmolarity plays an important part in perpetuating the “vicious circle” of inflammation and cell damage. The researchers correlated this condition with aqueous-deficient dry eye (in which hyperosmolarity decreases tear secretion) and evaporative dry eye (where hyperosmolarity is secondary to excessive evaporation). Using this knowledge, the researchers conducted a study to find which eye drops disrupt the hyperosmolar environment.
Five unique preservative-free lubricants—two available in the US (Optive and Systane) and three non-US brands—were compared to a control group and observed over a 15-minute period after application. A total of 150 patients (300 eyes) received treatment. The work was funded by Thea Pharma and included two of its international products (Hyabak and Siccafluid) in the study.
“All participants in this study were diagnosed with moderate to severe dry eye, identified by Ocular Surface Disease Index symptoms scoring 23 or higher and a baseline osmolarity of 308mOsm/L or more in one eye, or a variability of eight mOsm/L or more between both eyes,” mentioned the researchers in their study. Additionally, this study was conducted at the Dry Eye Unit of the San Diego Ophthalmology Clinic and each patient’s osmolarity was tested using the TearLab Osmolarity System.
According to the researchers, each lubricant showed a decrease in osmolarity 15 minutes after instillation; recorded post-treatment values ranged from 205mOsm/L to 285mOsm/L. The untreated control group registered a small increased in mean osmolarity of 0.98mOsm/L.
“It is crucial to emphasize that disrupting the hyperosmolar environment on the ocular surface can break the cycle of inflammation, damage to the microvilli of ocular surface cells, desiccation, and apoptosis, preventing the vicious circle that perpetuates dry eye,” reported the researchers in their paper for the Cornea journal. “This study is among the first to confirm that, at least as an immediate post-application effect, ocular lubricants can interrupt this vicious cycle by improving the hyperosmolar environment of the ocular surface.”
1. Stapleton F, Alves M, Bunya VY, et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15:334–365. 2. Muñoz EC, Patiño AO, Marín DJ, et al. Immediate impact on tear osmolarity following the application of different ocular lubricants in patients experiencing moderate dry eye symptoms. Cornea. March 15, 2024. [Epub ahead of print]. |


