 |
|
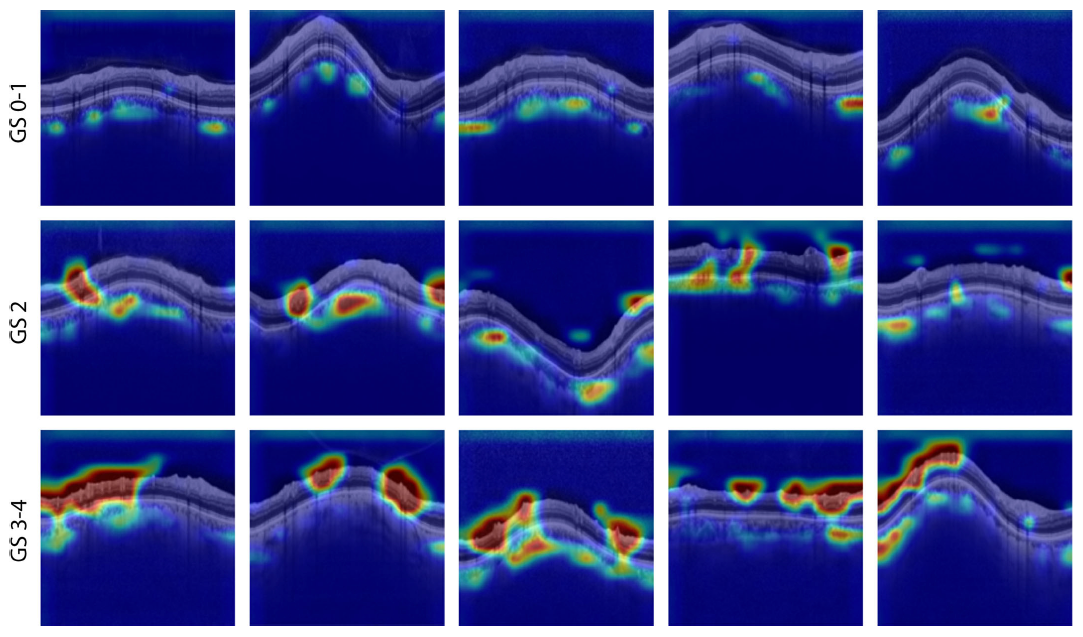
In the future, objective measures recorded with SD-OCT may help improve individualized glaucoma care by adjusting VF testing frequency based on deep-learning estimates of functional damage. In this image from the study, an AI technique called class activation mapping is used to highlight areas of peripapillary OCT scans that contribute to the patient’s visual performance as determined by standard automated perimetry (SAP). Examples of early (top row), moderate (middle) and advanced glaucoma (bottom) are shown. In time, the researchers believe, AI models will be able to predict VF status without need for the patient’s SAP data. Photo: Scandella D, et al. Transl Vis Sci Technol. 2024;13(6):10. Click image to enlarge. |
The “structure vs. function” debate in glaucoma and other ocular conditions might one day be collapsed into a single concept encompassing both, if emerging research bears fruit. One new study suggests it may in time be possible to reduce the frequency of visual field (VF) testing for glaucoma patients by using deep learning estimates of functional damage measured on spectral-domain OCT. In a new paper on AI efforts in glaucoma assessment, a research team from Switzerland explained, “It has now been shown that localized (glaucomatous) defects of the retinal nerve fiber layer (RNFL) can be recognized reliably using SD-OCT even before VF defects become apparent in perimetry.”
To see whether this method of VF assessment is reliable enough for clinical practice and how it stacks up against standard automated perimetry (SAP) in the objective prediction of VF performance, the team of researchers performed a retrospective observational study. Its methods and findings are described below.
The cohort included 5,238 unique eyes classified as suspects or diagnosed with glaucoma. All patients underwent ophthalmologic examination consisting of SAP, macular OCT and peripapillary OCT on the same day. Deep learning models were trained to estimate VF mean deviation and cluster mean deviation using retinal thickness maps from seven layers: RNFL, ganglion cell layer and inner plexiform layer (GCL + IPL), inner nuclear layer and outer plexiform layer, outer nuclear layer, photoreceptors and retinal pigmented epithelium, choriocapillaris and choroidal stroma and total retinal thickness.
The results showed that the deep learning models trained on retinal thickness maps and optic nerve head scans could accurately predict VF parameters in glaucoma patients, achieving better performance than the baseline linear regression model. Specifically, the RNFL, GCL + IPL and total retinal thickness achieved the best performance of all the retinal layers in predicting the mean deviation of the VF. Moreover, combining macular and optic nerve head scans improved the accuracy of mean deviation and cluster mean deviation prediction in glaucoma patients.
The performance of the deep learning model may also be influenced by the severity and stage of glaucoma, the researchers suggested. Their evaluation determined that the model performed best in predicting early and moderate glaucoma, but its effectiveness diminished notably in instances involving both glaucoma suspects and those with severe glaucoma.
A noteworthy limitation of this study is the reliance on automatically extracted layer segmentations to generate thickness maps, which may subject the model to segmentation errors. The researchers note in their paper that they plan to use unsegmented macular scans in a future investigation to eliminate this possibility.
“Accurate estimation of visual function from SD-OCT imaging can identify disease earlier and determine progression faster, enabling individualized VF testing frequency and reducing the overall need for VF tests,” the researchers summarized in their paper. “Deep learning models can estimate changes in VF results and postpone or recommend further testing, providing cost savings and standard metrics for monitoring patient visual function while reducing reliance on VF testing.”
The authors concluded that using their deep learning approach to extract relevant information from OCT images “could lead to new biomarkers for clinical decision-making and improve personalized patient care.”
Scandella D, Gallardo M, Kucur SS, Sznitman R, Unterlauft JD. Visual field prognosis from macula and circumpapillary spectral domain optical coherence tomography. Transl Vis Sci Technol. 2024;13(6):10. |


