 |
A 50-year-old female presented to the ophthalmic emergency department for foreign body sensation and pain OD for four days. She said her symptoms started after a cabinetry unit she had been holding slipped and forcefully hit her in the eye. She reported immediate pain and blurred vision. Since the accident, her pain and vision had improved; however, she was still experiencing persistent photophobia and headaches, which ultimately prompted her to seek care.
Case
On examination, her vision was 20/150 (pinhole 20/40) OD and 20/20 OS. Her intraocular pressures were 16mm Hg OD and 17mm Hg OS. The pupillary exam revealed pupils that were equal in size and no afferent pupillary defect. Her extraocular motilies were normal. Slit lamp examination revealed mild nasal injection in the right eye with a 4mm linear full-thickness corneal laceration nasally. The anterior chamber of the right eye had 1+ cell and 1-2+ pigment. There was a focal anterior cataract nasocentrally. The posterior segment exam was unremarkable, and no evidence of vitritis, intraocular foreign body or retinal damage was seen. The left eye exam was unremarkable.
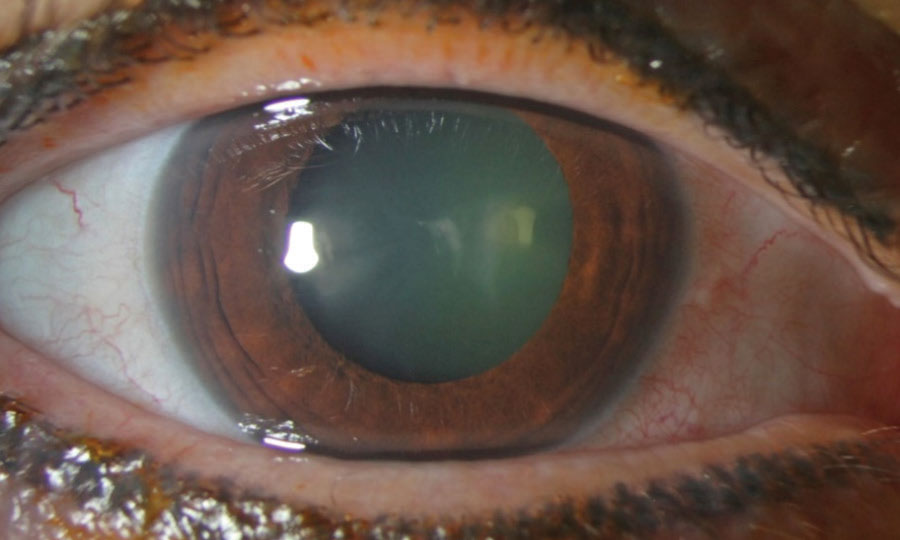 |
| This gross slit lamp photo reveals nasal conjunctival injection and a faint corneal opacity nasal to the center. There is also mild haze visible in the lens of the eye, where a focal cataract is present. Click image to enlarge. |
Given the full-thickness corneal laceration, signifying an open globe injury, it was important to conduct additional testing to fully understand the integrity of the globe. A Seidel test was completed by anesthetizing the eye and applying a wetted fluorescein strip directly over the wound under a blue light filter. There was no fluid emitting from the wound. Next, the test was repeated while applying gentle pressure to the globe to assess the wound’s stability under mild stress, which could be induced if the patient accidently rubbed the eye or when IOP was checked. The wound did not leak with provocation, signifying it had self-sealed. Corneal cross-section images revealed the beveled nature of the wound, likely explaining why the laceration did not leak.
In any case of open globe injury, a thorough examination of the eye and periocular structures is critical. In cases of polytrauma, blunt facial trauma or intraocular foreign body, computed tomography may be ideal.1 In this case, the posterior segment view was clear, and retinal trauma and intraocular foreign body could be ruled out. In cases that present with intraocular hemorrhage—either a hyphema and/or vitreous hemorrhage—and an obscured fundus view, it may be beneficial to obtain ocular ultrasonography to evaluate the interior of the eye.2 However, this should only be done by a provider who is very experienced using the technique, as further compression on the globe could cause other complications such as extrusion of intraocular contents or suprachoroidal hemorrhage.1
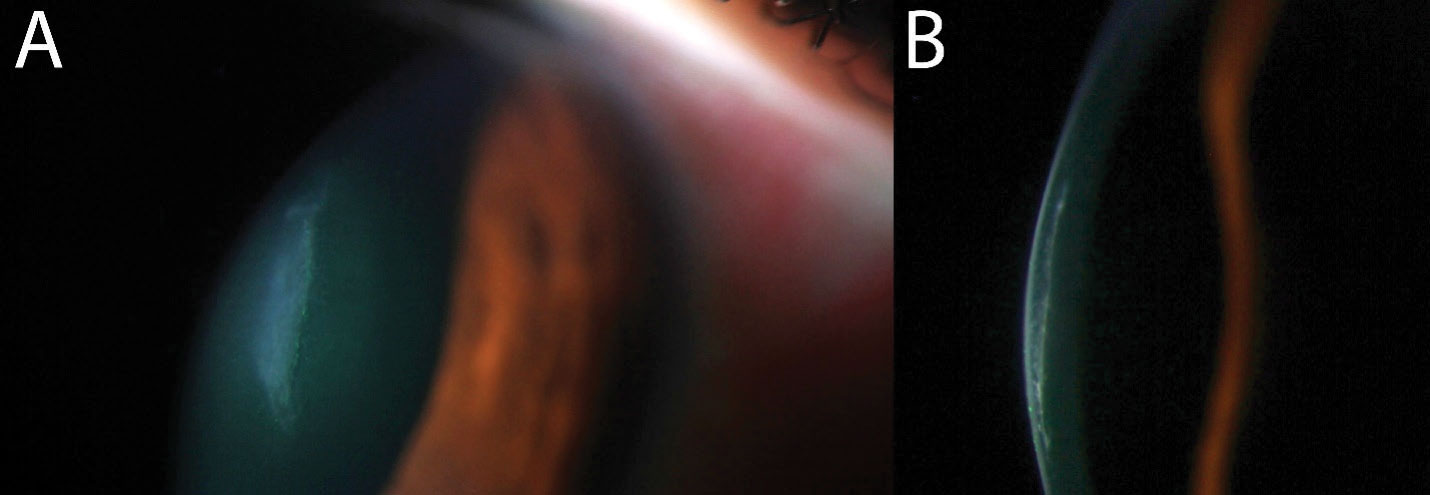 |
| A magnified view of the corneal laceration (A) with a dedicated cross-section shows the shelved nature of the laceration, likely allowing the wound to seal on its own (B). Click image to enlarge. |
Considerations
In our case, a major concern at this point was the development of an intraocular infection. Penetrating ocular trauma, intraocular surgery, intraocular injections and endogenous sources can all lead to infectious endophthalmitis.3 Post-traumatic causes alone make up about 25% to 30% of all cases of endophthalmitis.4 The risk of endophthalmitis in open globe injuries may be mitigated by administering a tetanus vaccine (particularly if the patient’s vaccination is not up-to-date and there was non-sterile trauma), systemic oral, intravitreal, intraocular or topical fortified antibiotics.5,6
Another concern with our patient was the risk of lens-induced inflammation, also known as a phacogenic or phacoanaphylactic reaction. This happens when lens proteins, believed to have immune privilege, are exposed to the rest of the intraocular structures. This occurs in only a few settings, such as a hypermature cataract with leakage of lens proteins through the capsule, incomplete removal of lens material during cataract surgery or after traumatic violation of the lens capsule.7 Phacogenic inflammation can lead to chronic uveitis, glaucoma, hyphema, corneal edema, vitritis or cystoid macular edema if not treated promptly.8 Management typically involves removing all inciting lenticular material and initiating topical anti-inflammatory agents.9,10 Vitrectomy may be performed in some cases to rule out infectious endophthalmitis or if lens material has migrated into the vitreous chamber.11
 |
| A small focal cataract is present, indicating penetrating ocular trauma. Click image to enlarge. |
Our patient was given oral levofloxacin in the emergency room on the day of her presentation, and fortified topical antibiotics, vancomycin and tobramycin were prescribed. She was also advised to start topical corticosteroids and mydriatic drops to minimize inflammation. Intravitreal antibiotics were not initiated at this point given the general lack of inflammation inside the eye. The patient was monitored closely over the following weeks and fortunately did not appear to have any increase in inflammation, pain or intraocular pressure. Cataract surgery was scheduled for one month later.
Since globe trauma increases the risk of any intraocular procedure, including cataract surgery, there are some important points to consider when planning for surgery and educating the patient on potential complications and outcomes. “Capsular integrity is of utmost importance when evaluating a patient with corneal perforation. We can assume capsular integrity is violated when cortical or lenticular material is found in the anterior chamber. Another clue is assessing for phacodonesis, as this may indicate direct trauma to the lens. An important point, however, is that it may be difficult to visualize these signs given the robust inflammation and corneal haze one may see on presentation,” says Zubair Ansari, MD, the surgeon in this patient’s case. “As a general rule of thumb, expect the unexpected when it comes to traumatic cataract. Traumatic cataracts tend to have higher rates of phacodonesis, vitreous prolapse and posterior capsular rupture.”
As far as educating the patient on postsurgical outcomes, Dr. Ansari notes that a thorough preoperative conversation about expectations is important given the higher risk of complications. These patients may often require a secondary or sulcus-placed intraocular lens, which can make refractive outcomes less predictable. Additionally, this particular patient had paracentral irregular corneal astigmatism that would likely lead to decreased visual quality even after the cataract was removed. Since the astigmatism was non-central and irregular, a toric or multifocal lens was not appropriate. The patient underwent a carefully performed cataract surgery, in which the anterior capsular violation was incorporated into the capsuolorhexis, and a standard monofocal lens was placed in the capsule. She was advised to consider a rigid gas permeable contact lens after surgery for the best visual outcome.
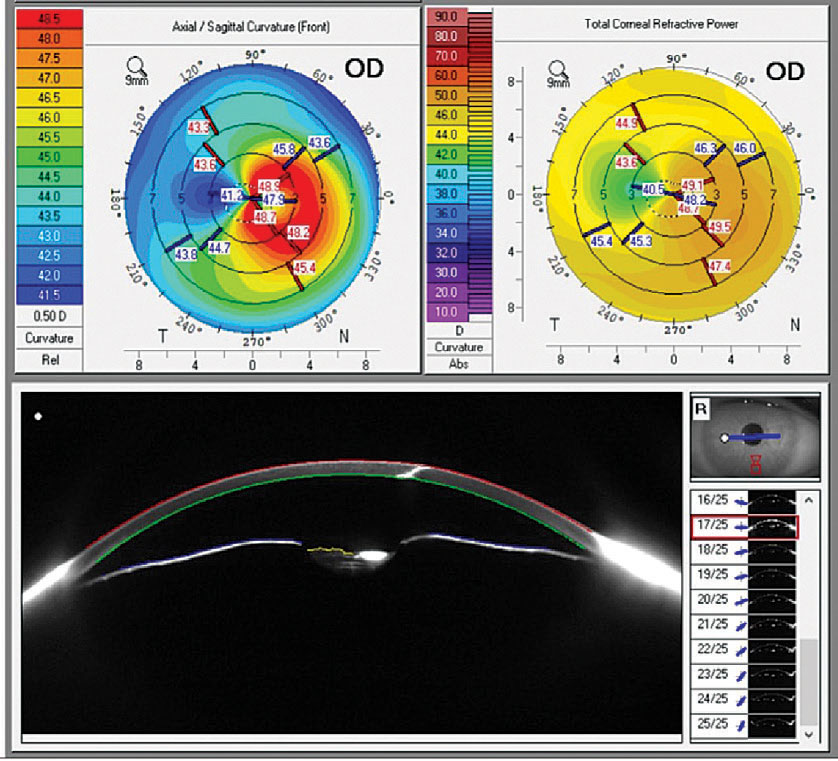 |
| Corneal topography and anterior segment Scheimpflug imaging reveal the irregular corneal astigmatism affecting the visual axis (top) and the full-thickness corneal laceration, seen as a hyper-reflective cut through the cornea (bottom). Click image to enlarge. |
Takeaways
This case highlights the importance of a careful examination of all parts of the eye in ocular trauma. Penetrating ocular traumas can present with severe or minimal-appearing injuries, but they all carry an elevated risk of infection and potential complications. Our job as primary eyecare doctors is to fully document the eye’s initial status, limit and carefully watch for complications and educate patients on potential risks and outcomes. With prompt and thorough care, many patients can still obtain favorable visual outcomes.
Dr. Bozung works in the Ophthalmic Emergency Department of the Bascom Palmer Eye Institute (BPEI) in Miami and serves as the clinical site director of the Optometric Student Externship Program as well as the associate director of the Optometric Residency Program at BPEI. She has no financial interests to disclose.
|
1. Bodanapally UK, Saeedi O. Reply. AJNR Am J Neuroradiol. 2017;38(11):e101. 2. Lecler A, Pinel A, Koskas P. Open globe injury: ultrasound first! AJNR Am J Neuroradiol. 2017;38(11):e99-100. 3. Simakurthy S, Tripathy K. Endophthalmitis. In StatPearls. 2022: Treasure Island (FL). 4. Bhagat N, Nagori S, Zarbin M. Post-traumatic infectious endophthalmitis. Surv Ophthalmol. 2011;56(3):214-51. 5. Abouammoh MA, Al-Mousa A, Gogandi M, et al. Prophylactic intravitreal antibiotics reduce the risk of post-traumatic endophthalmitis after repair of open globe injuries. Acta Ophthalmol. 2018;96(3):e361-5. 6. Ahmed Y, Schimel AM, Pathengay A, et al. Endophthalmitis following open-globe injuries. Eye (Lond). 2012;26(2):212-7. 7. Sridhar U, Tripathy K. Lens induced inflammation. In StatPearls. 2022: Treasure Island (FL). 8. Nche EN, Amer R. Lens-induced uveitis: an update. Graefes Arch Clin Exp Ophthalmol. 2020;258(7):1359-65. 9. Marak GE Jr. Phacoanaphylactic endophthalmitis. Surv Ophthalmol. 1992;36(5):325-39. 10. Shah SS, Meyer JJ. Lens induced glaucoma. In StatPearls. 2022: Treasure Island (FL). 11. Imen K, Tahar Meriam BH, Ilhem S, et al. Lens-induced hypopyon uveitis as the presenting manifestation of posterior lens nucleus dislocation following pars-plana vitrectomy: case report. J Ophthalmic Inflamm Infect. 2021;11(1):42. |

