 |
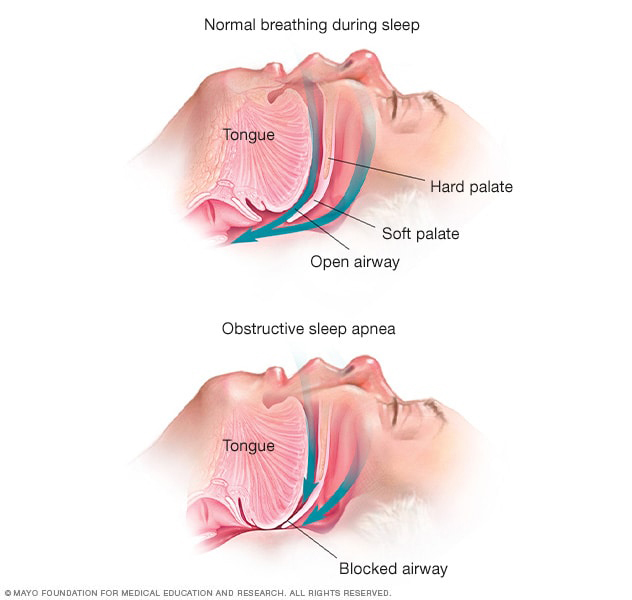
CPAP used for OSA treatment remains unclear in providing a positive or negative effect on glaucoma progression. Photo: Mayo Clinic. Click image to enlarge. |
Research published in Eye sought to clarify the connection between sleep apnea and glaucoma since previous studies on the topic have been conflicting. Since many newer studies have been published, the study researchers conducted a meta-analysis of obstructive sleep apnea (OSA) and glaucoma association.
A total of 48 studies were included from multiple databases in the systematic review with 46 of those suitable for meta-analysis. The total study population included 4,566,984 patients. The researchers found a higher glaucoma risk for those with OSA. After adjusting for various confounding factors, including age, sex and comorbidities of hyperlipidemia, hypertension, cardiovascular disease and diabetes, 40% higher odds of glaucoma were determined in OSA patients.
The researchers also included separate information about OSA’s effects on nonglaucomatous eyes, such as quantifiable markers of glaucomatous change in the eye, looking at characteristic visual field defects, intraocular pressure (IOP) and retinal nerve fiber layer (RNFL) thickness. They found that OSA patients experienced more significant visual field loss when compared with those without the condition. These patients also saw higher IOP and thinner RNFL thickness, potentially indicating more advanced disease. Severe OSA displayed the highest IOP and thinnest RNFL.
The researchers proposed multiple factors that may contribute to the underlying pathophysiology resulting in this association, including hypoxic damage, vascular changes and mechanical factors.
Hypoxic changes may result from OSA sleep fragmentation, raising sympathetic drive and increasing systemic inflammation and immune dysregulation. Otherwise, repetitive apnea-hypopnea episodes could damage the optic nerve head, retinal ganglion cells and their axons, thus leading to glaucoma.
As for mechanical changes, raised IOP at night with OSA may contribute to glaucoma progression. This is due to raised episcleral venous pressure that has been suggested as an explanation when laying in a supine position.
The authors mentioned that OSA treatment, mainly CPAP, still remains uncertain in its effects and interplay with glaucoma. They cited that one study suggests CPAP treatment improves ocular parameters associated with glaucoma progression, including IOP and RNFL thickness.
Previous research, however, negates this finding, with observations pointing to increased IOP with CPAP use at night. This counterevidence is hypothesized to be due to increased intrathoracic pressure seen with CPAP usage.
Although sleep apnea treatment may not be concretely determined to either help or hinder glaucoma progression, the authors provided other suggestions for practicing clinicians.
“Given the large number of OSA cases which go undiagnosed and untreated, it is important for clinicians to be cognizant of a possible association between these two conditions. A multidisciplinary approach involving both sleep clinicians and ophthalmologists may be ideal for optimizing care for patients diagnosed with either condition or both.”
As a final note, the authors believe that “patients with OSA, especially those with severe sleep apnea, may benefit from regular ophthalmic examination to pick up asymptomatic or early cases of glaucomatous disease.”
Cheong AJY, Wang SKX, Woon CY, et al. Obstructive sleep apnoea and glaucoma: a systematic review and meta-analysis. Eye (Lond). March 28, 2023. [Epub ahead of print]. |

