 |
Q:
Pregnancy can affect the corneal thickness and intraocular pressure (IOP) of women, impeding proper LASIK screening and complicating glaucoma diagnosis and treatment. What management protocol exists for women who may be experiencing transient corneal effects during pregnancy?
“A recent paper published in BMC Ophthalmology has reopened the conversation about the effects of female sex hormones on the cornea throughout a woman’s life cycle,” notes Suzanne W. Sherman, OD, an associate professor at University of South Florida. Specifically with corneal changes that occur during pregnancy, the question has been brought up of what standards to follow.1
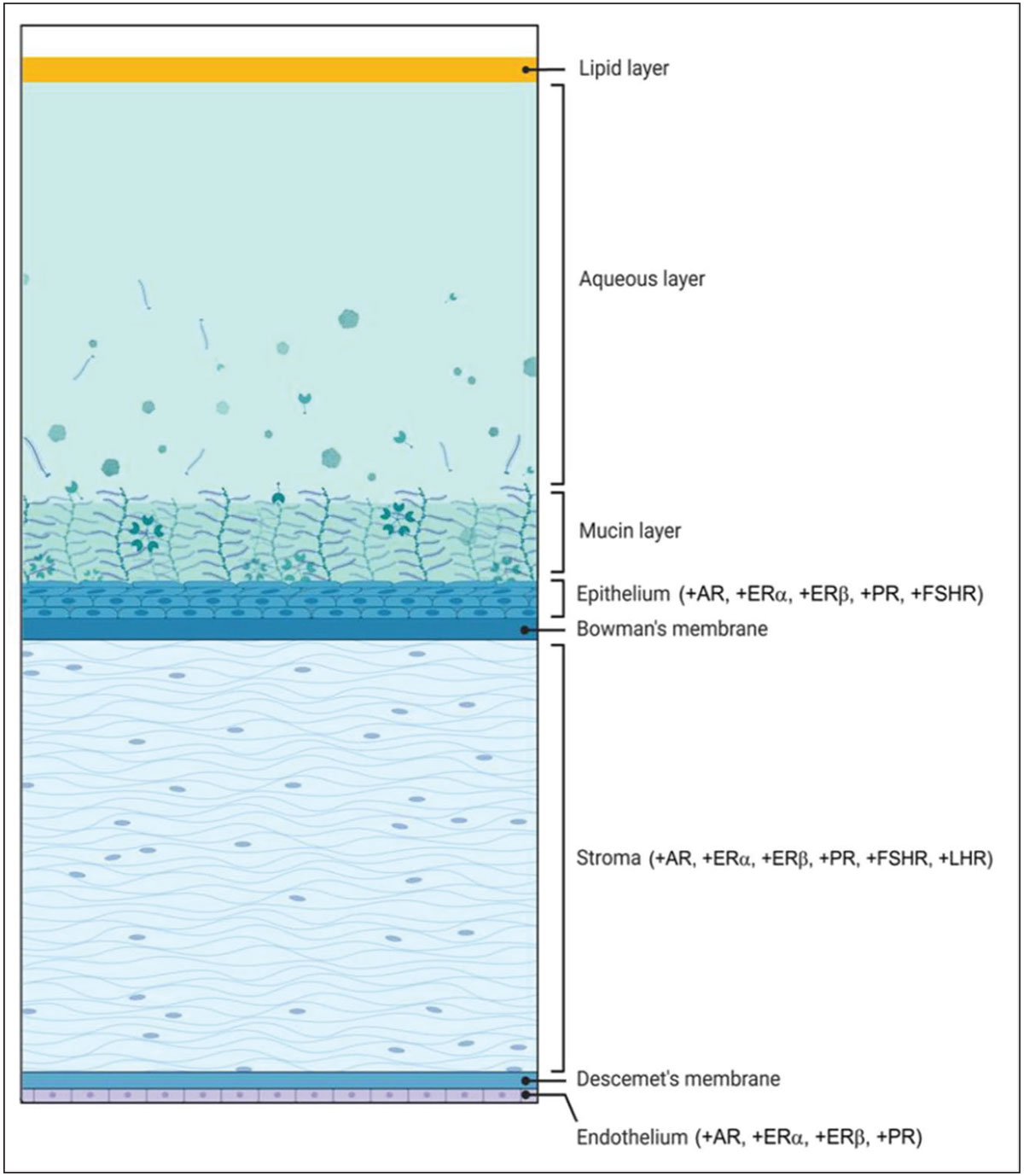
The article confirmed that increases in corneal curvature and thickness are due to corneal edema in pregnancy, which can be a factor in transient visual symptoms. These changes are thought to be caused by fluid retention, progesterone and estrogen receptors in the stroma and increased collagenolytic activity. A separate study by Weinreb et al. also reported an increase in corneal thickness, corneal volume and decreased keratometry values.2,3
Unintended Changes
“These corneal changes primarily affect refractive error and can contribute to IOP and keratoconus alterations,” Dr. Sherman explains. However, refractive error changes that were caused by corneal thickness and volume alterations were not found statistically significant by Weinreb et al. As such, there is varying opinion on whether to prescribe glasses or contact lenses for pregnant patients with fluctuating visual symptoms. A review by Morya et al. stated that glasses prescribed while pregnant may become irrelevant postpartum due to a myopic shift.4 In contradiction, Weinreb et al. state pregnancy is not a contraindication for prescribing corrective lenses.2,4
Thus, no established protocol has been set, but if the patient is symptomatic and a change in manifest refraction is found, educating the patient on the possibility of a refractive shift postpartum is important, Dr. Sherman establishes.5
 |
|
At left, diagram illustrating the cornea’s hormonal receptors. AR: androgen receptor; ER: estrogen receptor; PR: progesterone receptor; LHR: luteinizing hormone receptor; FSHR: follicle-stimulating hormone receptor. A plus sign (+) indicates evidence of receptor or enzyme mRNA expression in that respective layer. Reproduced under Creative Commons 4.0 license from Kelly DS, Sabharwal S, Ramsey DJ, Morkin MI. The effects of female sex hormones on the human cornea across a woman’s life cycle. BMC Ophthalmol. 2023;23:358. Click image to enlarge. |
Another reason a patient may report new-onset visual symptoms during pregnancy is due to an underlying diagnosis of keratoconus, she adds. One study found a decrease in Goldmann and corneal-compensated IOP measurements in pregnant women with keratoconus that lasted until six months post-partum.6 This further suggests the importance of screening and discussing corneal crosslinking with keratoconus patients before conception, as well as continuous screening during pregnancy and postpartum.
When looking at pregnant patients, many studies have established that IOP changes in the second trimester, with pregnant women experiencing lower IOP than non-pregnant patients. This is due to an increase in outflow facility via increased uveoscleral outflow, decreased episcleral venous pressure and scleral rigidity, acidosis during pregnancy and the accompanying increase in corneal thickness, elucidates Dr. Sherman. A decrease in IOP around 10% (2mm Hg to 3mm Hg) is seen in the second half of pregnancy.2,5
The World Glaucoma Association has set guidelines that recommend targets for providers to use based on their patient’s glaucoma severity, as this factor determines the aggressiveness of treatment. It recommends the following IOP limits to providers to decide whether to modify treatment: 35mm Hg for mild glaucoma, 30mm Hg for moderate and 25mm Hg for advanced. After 20 weeks, these targets change to 30mm Hg for mild, 25mm Hg for moderate and 20mm Hg for advanced glaucoma. Despite IOP dropping during pregnancy, it has been suggested that glaucoma during pregnancy can result in progressive field loss with up to 17.9% of patients experiencing loss.5,7,8 Depending on the severity, these patients should be followed every one to three months.
Currently, a specific protocol for prescription changes due to transient corneal effects during pregnancy does not exist, Dr. Sherman states. “It is up to the provider to educate the patient and collaboratively conclude if a new prescription is necessary. In terms of transient corneal effects that can alter the course of patients’ glaucoma or keratoconus, increased screening is recommended, and the frequency of this assessment will depend on the severity of the patient’s condition,” she concludes.
Dr. Shovlin, a senior optometrist at Northeastern Eye Institute in Scranton, PA, is a fellow and past president of the American Academy of Optometry and a clinical editor of Review of Optometry and Review of Cornea & Contact Lenses. He consults for Kala, Aerie, AbbVie, Novartis, Hubble and Bausch + Lomb and is on the medical advisory panel for Lentechs.
1. Kelly DS, Sabharwal S, Ramsey DJ, Morkin MI. The effects of female sex hormones on the human cornea across a woman’s life cycle. BMC Ophthalmol. 2023;23:358. 2. Weinreb RN, Lu A, Beeson C. Maternal corneal thickness during pregnancy. Am J Ophthalmol. 1988;105(3):258-60. 3. Millodot M. The influence of pregnancy on the sensitivity of the cornea. Br J Ophthalmol. 1977;61(10):646-9. 4. Morya AK, Gogia S, Gupta A, et al. Motherhood: what every ophthalmologist needs to know. Indian J Ophthalmol. 2020;68(8):1526-32. 5. Sherman SW. Pregnancy and postpartum ophthalmic changes can present a challenge. Optometry Times. 2022;14(2). 6. Naderan M, Jahanrad A. Topographic, tomographic and biomechanical corneal changes during pregnancy in patients with keratoconus: a cohort study. Acta Ophthalmol. 2017;95(4):e291-6. 7. Khong EWC, Chan HHL, Watson SL, Lim LL. Pregnancy and the eye. Curr Opin Ophthalmol. 2021;32(6):527-35. 8. Weinreb R, Grajewski A, Papadopoulos M, et al. Medical treatment of glaucoma: the 7th Consensus Report of the World Glaucoma Association. Fort Lauderdale, Florida: Kugler Publications. 2010. |

