 |
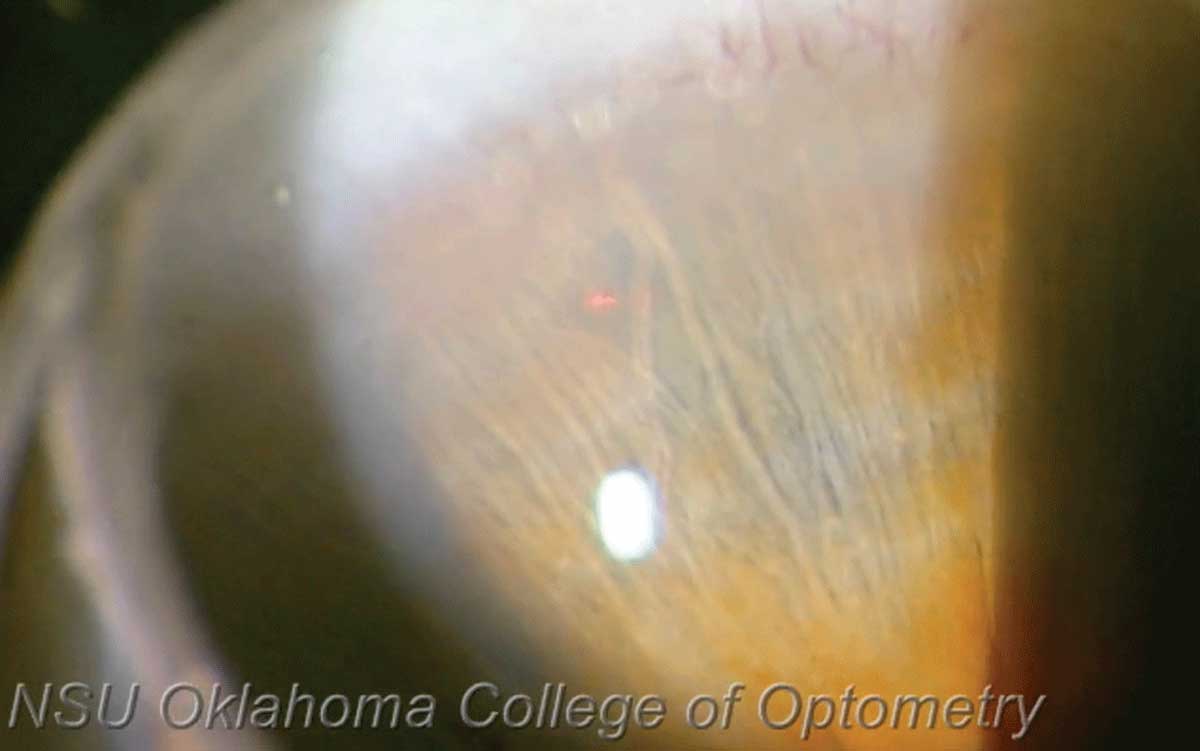
| The short-term angle-widening effect of LPI in patients with PACD was found to be limited, with even this small effect on the anterior chamber angle decreasing over time. Photo: Joseph Shetler O,D, and Nathan Lighthizer, OD. Click image to enlarge. |
Laser peripheral iridotomy (LPI) remains a first-line treatment option to resolve pupillary block in patients with primary angle closure disease (PACD), subsequently reducing the iridotrabecular contact and widening the anterior chamber angle, which is comprised of the iris, trabecular meshwork and cornea. A recent study in American Journal of Ophthalmology longitudinally evaluated a cohort of patients with PACD who underwent LPI for a relatively long follow-up period, with the intention of investigating age-related anterior segment changes associated with anterior chamber angle status through serial images obtained by the same AS-OCT device. The research team, based in South Korea, noted that changes in anterior segment parameters affected anterior chamber angle in complex patterns. In particular, the lens vault continues to increase after LPI, accompanied by progressive narrowing of the anterior chamber angle. So, the researchers proposed that appropriately timed lens extraction could be important for clinical management of PACD to avoid synechial angle closure.
The study included 103 patients who visited the glaucoma clinic with PACD who underwent LPI and were followed-up by a mean 6.7 AS-OCT examinations for a mean 6.5 years. PACD was diagnosed based on the results of gonioscopic examination. Primary angle closure suspect (PACS) was diagnosed when an eye had an occludable angle, in which the pigmented posterior trabecular meshwork was not visible on nonindentation gonioscopy for at least 180º in the primary position, in the absence of elevated IOP or peripheral anterior synechiae (PAS). PAC was defined as IOP >21mm Hg or PAS formation in PACS. Participants were included if (1) they were followed-up for at least four years, (2) at least four serial qualified AS-OCT images were obtained every six to 12 months at the discretion of the clinician, and (3) they underwent LPI in either superotemporal or superonasal quadrant during the follow-up period.
Multivariate linear mixed effects models showed that decrease in angle opening distance was not significant (-1.59μm/yr); however, angle recess area decreased over time (-2.3 × 103μm2/yr) and scleral spur angle showed marginal significance (-0.20°/yr). Lens vault increased significantly (11.6μm/year) after LPI. Mean lens vault change was negatively associated with angle opening distance, angle recess area and scleral spur angle, while pupil diameter was negatively associated with angle recess area. Pupil diameter decreased with aging (-13.7μm/year) accompanied by thinning of iris thickness (-1.7μm/year).
“A longitudinal study including individuals with and without PACD could determine the nature of age-related changes in lens vault and whether these trends are affected by PACD,” the researchers wrote in their paper. “Differences in the temporal trends of lens vault changes in eyes with and without PACD would suggest that lens vault change is one of the core mechanisms in the development of angle closure and could possibly aid in predicting the long-term risk of angle closure in individuals.”
“Further studies investigating the relationships between age-related anterior segment changes, glaucomatous structural and functional progression or IOP change, and anterior chamber angle are warranted in this context,” the study concluded.
Kwak J, Shon K, Lee Y, Sung KR. Progressive changes in the anterior segment and their impact on the anterior chamber angle in primary angle closure disease. Am J Ophthalmol. August 25, 2023. [Epub ahead of print]. |

