 |
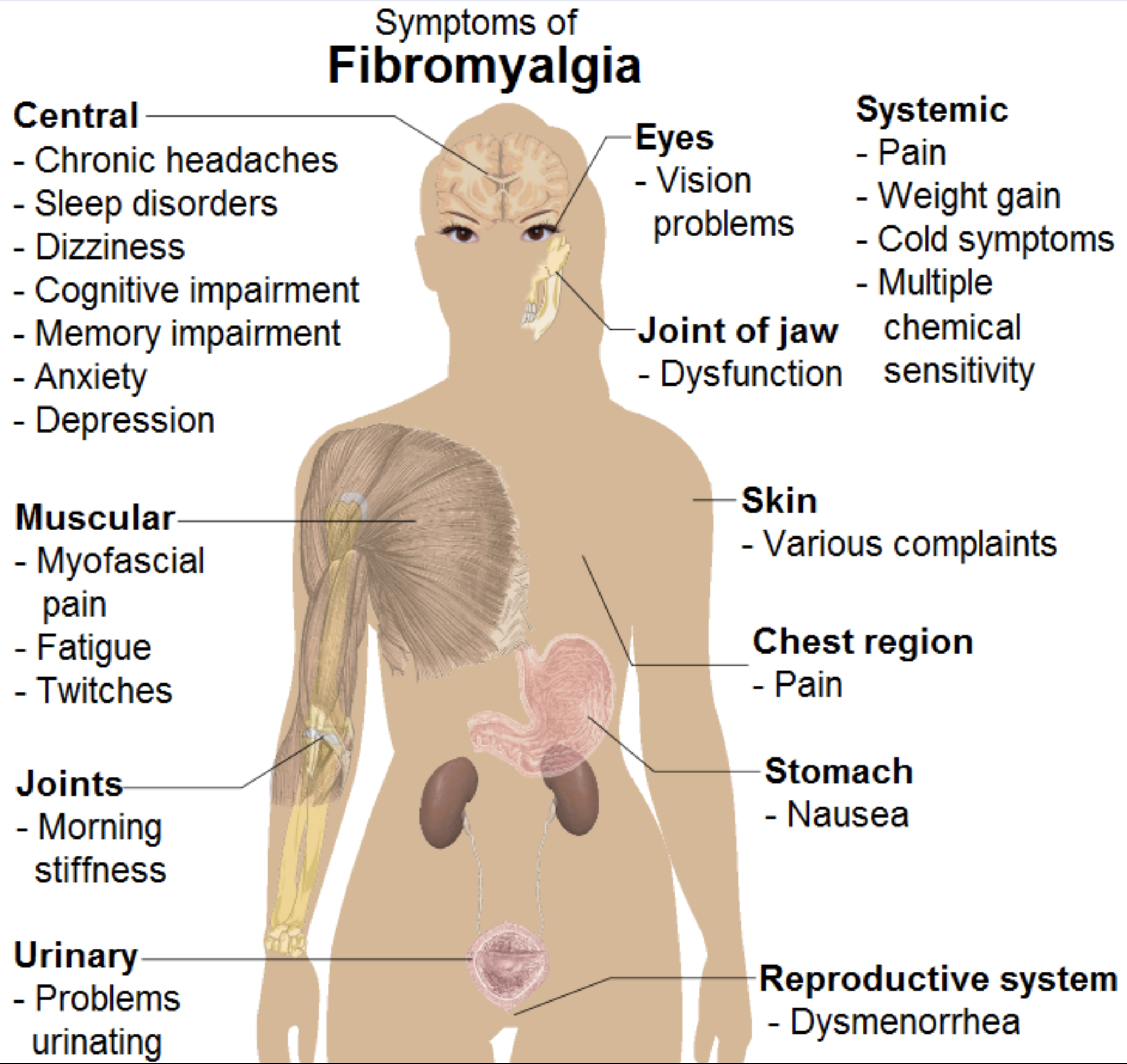
| Fibromyalgia and optic neuritis likely share a pathophysiology of autoimmunity-related neuroinflammation. Photo: Wikimedia Commons. Click image to enlarge. |
Editor’s Note: As part of our “Year in Review” retrospective, we’ve selected the top 30 news stories of the year and are re-sharing them as we close out 2023. Follow along as we count down to number 1!
This story was originally published September 1, 2023.
No. 6 biggest news story of 2023
Fibromyalgia is a fairly prevalent but poorly understood condition, and its ocular involvement is even less well defined. In a recent study on the topic conducted in Korea, researchers divided participants aged 20 to 79 into those diagnosed with fibromyalgia and those with pain but no diagnosis of fibromyalgia. Both groups contained 479,892 participants (median age 45).
During the study period, new incident optic neuritis cases were seen in 663 patients with fibromyalgia and 311 patients without fibromyalgia. Optic neuritis developed at a mean age of 54 and 52 years in the fibromyalgia and non-fibromyalgia groups, respectively.
Overall, the fibromyalgia group had an optic neuritis incidence rate of 35.65 per 100,000 person-years, compared with 16.75 per 100,000 person years in the non-fibromyalgia group. The fibromyalgia group also had a significantly higher hazard ratio than the non-fibromyalgia group. Mean time to incident optic neuritis from fibromyalgia onset was 2.4 years.
Additionally, the researchers reported that optic neuritis risk significantly increased in men between 60 and 79 years of age, and in women between 20 and 39 years of age. They attributed these differences to the effects of sex hormones and immune reactions, explaining that men have increased overall inflammation in old age due to declining levels of testosterone, while women with fibromyalgia often have growth hormone deficiencies, leading to a decrease in estrogen production in early adulthood that would otherwise protect against neuroinflammation until menopause-related declines.
"Since the autoantibody in fibromyalgia has not yet been fully elucidated and is still being studied, it is assumed that various immune mechanisms exist between fibromyalgia and the optic nerve, which consequently contribute to the neuroinflammation of the optic nerve,” the researchers wrote in their American Journal of Ophthalmology paper.
“Based on our results, older men and younger women diagnosed with fibromyalgia should be followed up for the development of optic neuritis,” the researchers concluded. “From a prevention perspective, regular ophthalmic examination and active control of any inflammatory reactions may be helpful in preventing or detecting this complication in its early stages in fibromyalgia patients.”
Cho H, Lee G, Lee J. Increased risk of optic neuritis in patients with fibromyalgia: nationwide population-based cohort study in South Korea. Am J Ophthalmol 2023. [Epub ahead of print]. |

