 |
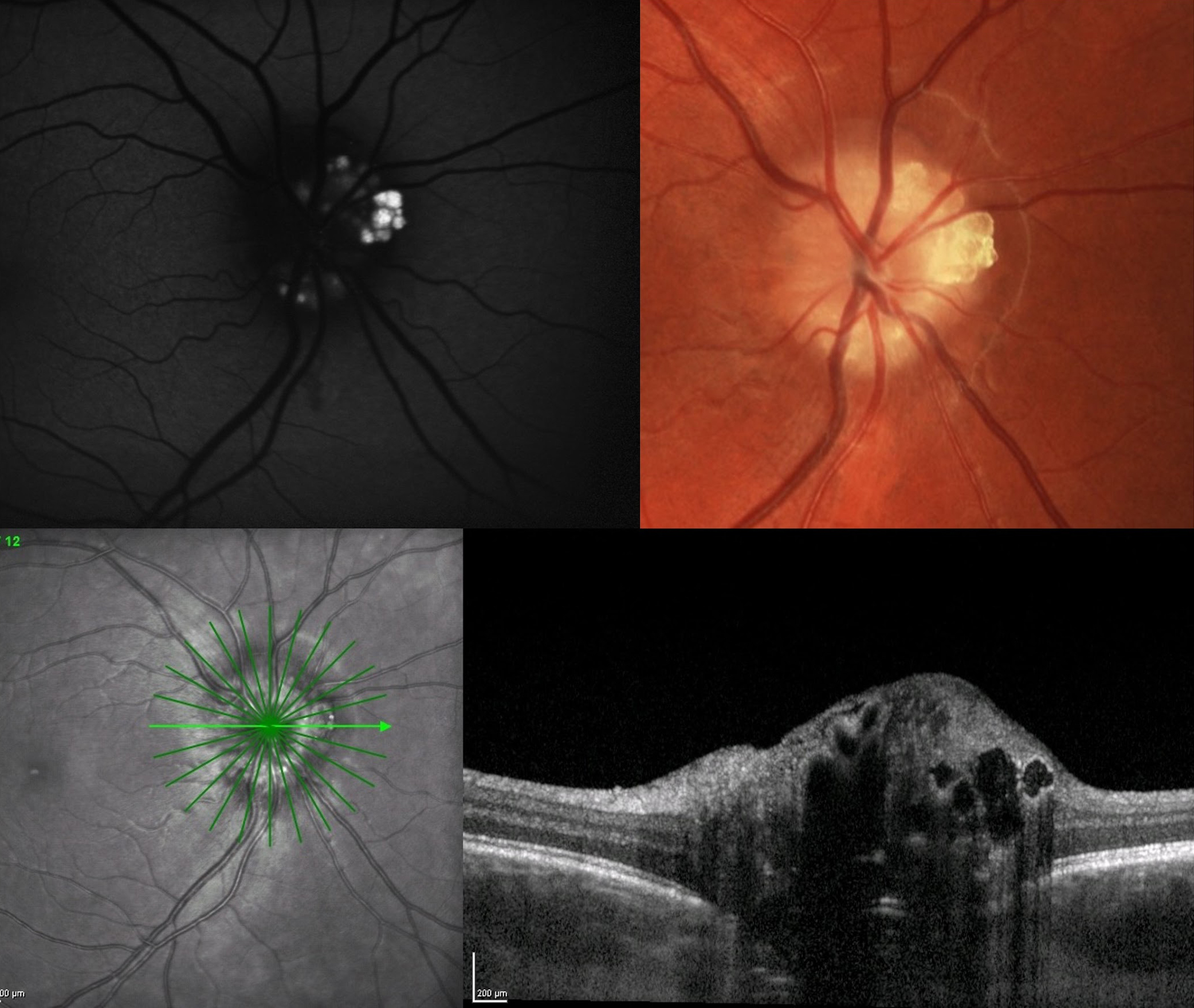
| Future studies should strive to employ EDI-OCT to obtain a full phenotype involved in combined ODD and RP. Photo: Jessica Haynes, OD. Click image to enlarge. |
Identification of the calcified optic nerve deposits that comprise optic disc drusen (ODD) is sometimes a cause for concern, though the condition is known to be present in about 2% of the general population. However, a new study using enhanced-depth imaging OCT (EDI-OCT) finds a far higher rate in patients with retinitis pigmentosa (RP) than previously known, at 30%, according to a paper published in Journal of Neuro-Ophthalmology.
Included in the study were 40 patients with RP over the age of 18. All underwent an ophthalmic examination, including kinetic perimetry, EDI-OCT of the optic nerve head and fundus photography. Genetic testing was also conducted with a next-generation sequencing panel of retinal dystrophy genes. At least one ODD was found in 30%, or 12 patients; six subjects displayed bilateral ODD. There were no differences seen in those with and without ODD according to age, refraction, best-corrected visual acuity, Bruch’s membrane opening or visual field. Genetic variation causing RP was found in 11 of 12 cases of those with ODD and in 17 of 28 cases in the group without.
Previous reports indicate ODD prevalence in RP patients to be between 2% and 7% using fundus photography and fundus autofluorescence. This may have been much lower than the present study because of small heterogenous study populations and the lack of EDI-OCT use. In this study, only 39% of eyes with ODD were identified using fundus photography and 33% with fundus autofluorescence. In previous reports using EDI-OCT as a diagnostic method, the researchers found similar increase in ODD prevalence. Because the 30% prevalence of ODD seen in RP patients is 15 times higher than in the general population and much higher than estimated in prior studies, the study authors contend for a potential “indicating that the two conditions might be pathogenically related.”
The only parameter that differed between those with vs. without ODD was the prelaminar hyperreflective lines. All RP patients with ODD had hyperreflective lines but this was only present in 46% of those without ODD. This percentage is much greater than the percentages ranging from 3.4% to 12.3% in normal individuals and the reason for the high number is unknown. The authors do speculate that this could indicate an unfulfilled potential for ODD development in the given cases, as hyperreflective lines have been shown to represent potential ODD precursors.
Even more, since only half the patients displayed unilateral ODD, it remains to be seen if this could be possible due to local ocular factors as opposed to a monogenetic germline cause. Upon further examination, 83% of unilateral cases were classified as small and 67% of patients with unilateral ODD had hyperreflective lines present in the opposite eye, suggesting whatever underlying factor responsible for ODD development may affect both eyes to a degree.
In terms of the genetic testing, the variants responsible for RP were found in many genes in both ODD and no ODD groups. In their paper, the authors explain that “in both groups, the gene function included ciliary transport, the phototransduction cascade and the visual cycle. This speaks against ODD having a monogenetic cause related to genes causing RP. However, multiple genetic factors and other factors, such as those associated with retinal degeneration, could potentially be involved and contribute to a multifactorial etiology.”
Steensberg AH, Schmidt DC, Malmqvist L, et al. Optic disc drusen prevalence in patients with retinitis pigmentosa: a cross-sectional study. J Neuroophthalmol. November 17, 2023. [Epub ahead of print]. |

