 |
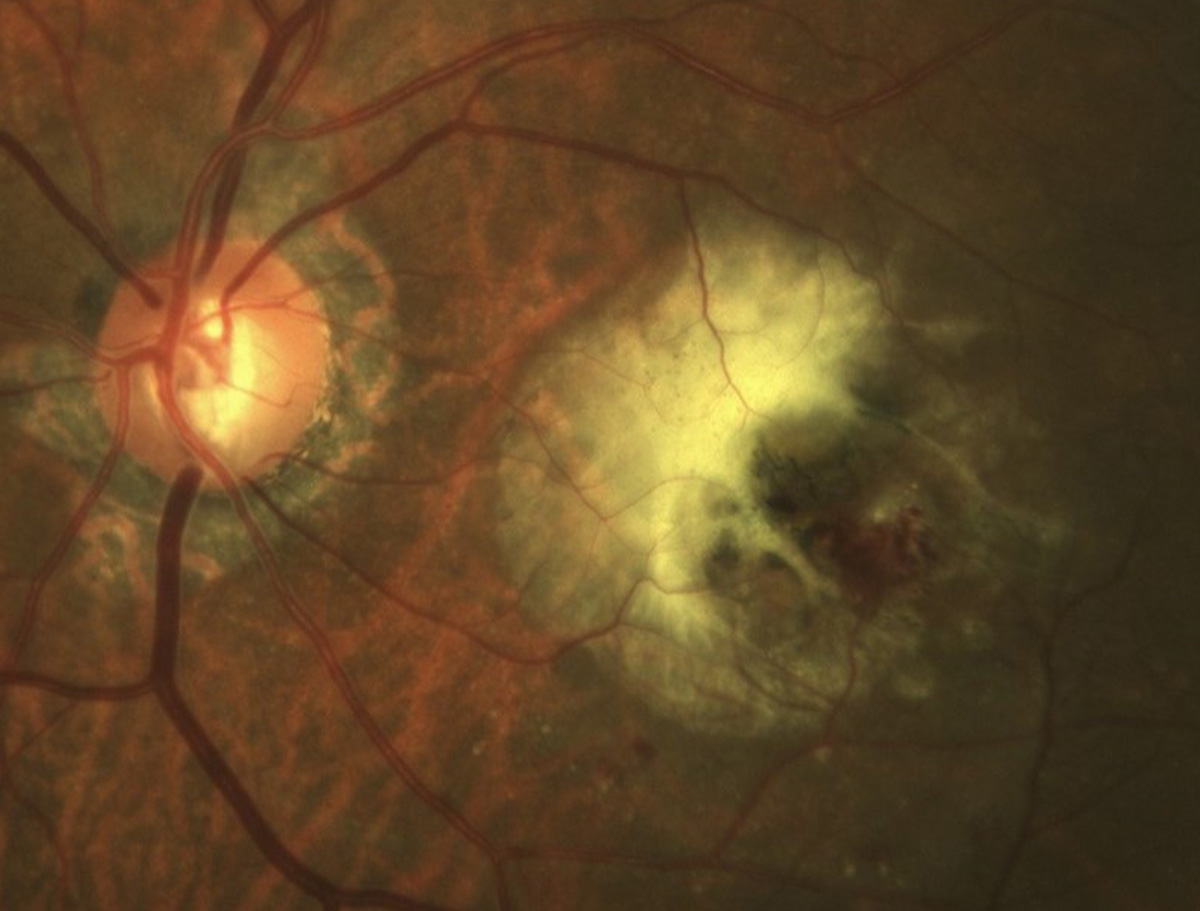
Type 3 macular neovascularization (also known as retinal angiomatous proliferation) involves progression from intraretinal vascularization to subretinal neovascularization and then choroidal neovascularization. Reports show it’s more common in female patients. Photo: Mohammad Rafieetary, OD. Click image to enlarge. |
It’s long been thought that type 3 macular neovascularization is more difficult to treat than other nAMD subtypes, in part, researchers say, due to a lack of large-scale randomized controlled trials. To investigate, a team from the UK and Italy evaluated three-year retrospective real-world data on patient outcomes and found that (similar to previous reports) while anti-VEGF conferred some benefits, vision returned to baseline in the long-run, and other disease developments do suggest that this form of nAMD is more severe.
The review included 59 eyes of 48 British patients with type 3 macular neovascularization who had received anti-VEGF intravitreal injections between 2013 and 2020. Best-corrected visual acuity and central macular thickness were the primary outcomes. Secondary outcomes included development of new-onset foveal-involving geographic atrophy and disciform scars.
The researchers reported that anti-VEGF treatment conferred a statistically significant reduction in central macular thickness during the 36-month study period. A total of 24 eyes demonstrated >50 µm reduction in central macular thickness and seven eyes remained stable. Two eyes experienced an increase in central macular thickness >50 µm vs. baseline.
By the third year of the study, slightly more than half of eyes showed evidence of deterioration but 47% of eyes remained stable or improved. Despite this, there wasn’t a statistically significant difference between median best-corrected visual acuity and baseline. New onset macula-involving atrophy or scarring was found in 10.2% and 4.3% of eyes, respectively.
The researchers concluded that this long-term, real-world data is a valuable addition to the body of research on anti-VEGF treatment for type 3 macular neovascularization. Additionally, they explained that patients with type 3 macular neovascularization are at high risk for macular atrophy. “Pre-existing thin choroid and reduced choriocapillaris flow may limit the response to increased VEGF expression and be a risk factor of onset or progression of atrophy,” the researchers wrote in their Eye paper. “Reduced choroidal flow due to atrophy appears to precede abnormal neovascularization and treatment with anti-VEGF intravitreal injections may revert the retina to its previous atrophic state.” They added that reports have shown that “nascent geographic atrophy may actually predict the development of type 3 macular neovascularization.”
Xue CC, Sim R, Chee ML, et al. Is kidney function associated with age-related macular degeneration? Findings from the Asian Eye Epidemiology Consortium. Ophthalmology. December 29, 2023. [Epub ahead of print]. |

