 |
|
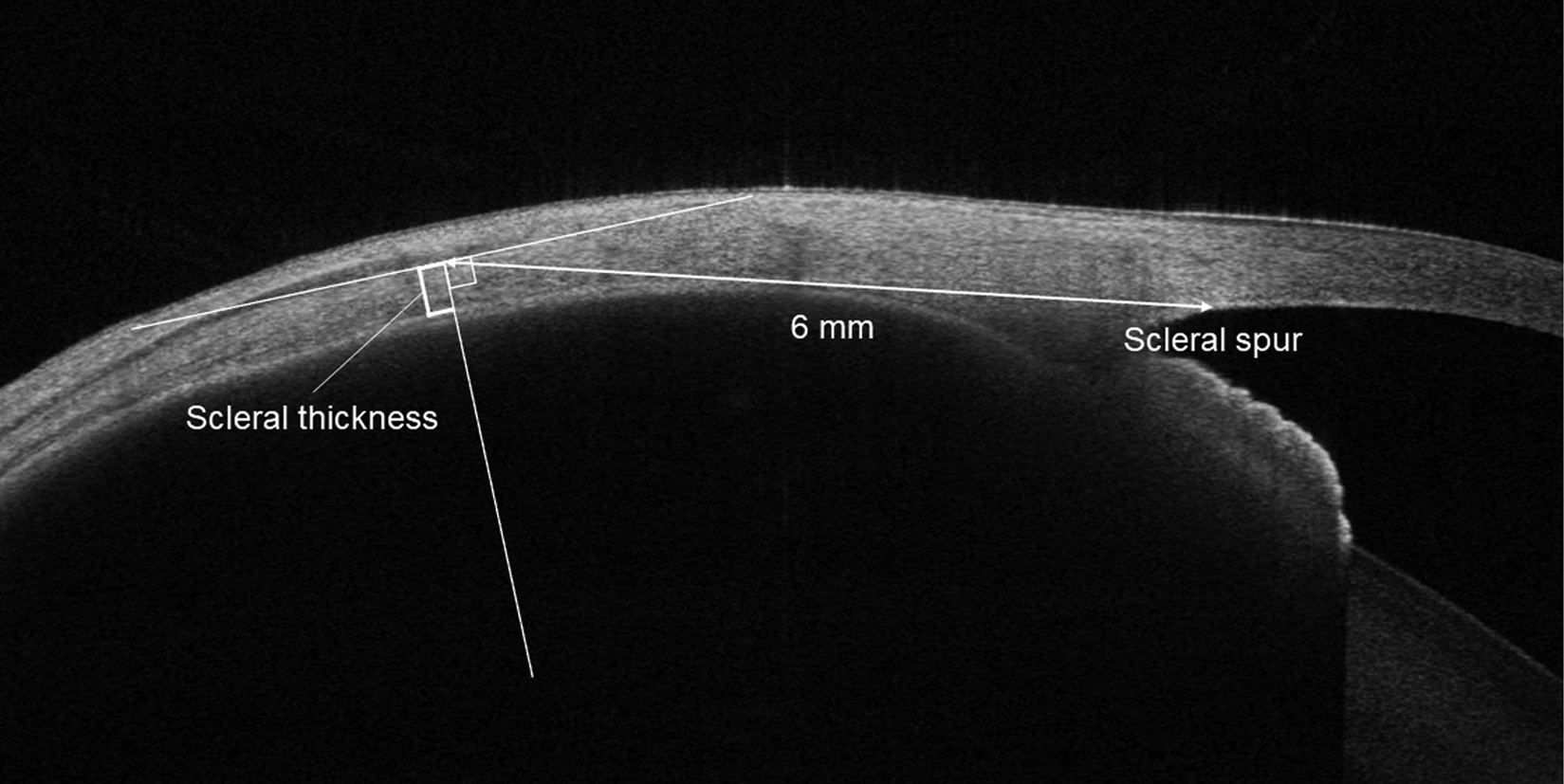
Researchers observed that complex central serous chorioretinopathy cases were more significantly associated with scleral thickening (measured here using anterior segment OCT), persistent subretinal fluid, outer retinal atrophy and intraretinal fluid. Photo: Imanaga N, et al. American J Ophthalmol. Jan 22, 2024. Click image to enlarge. |
Traditionally, central serous chorioretinopathy (CSCR) has been categorized as acute or chronic, but a recent rethinking by the Central Serous Chorioretinopathy International Group has led to a new multimodal imaging-based classification of these cases as simple or complex. After publicly releasing the proposal, researchers from Japan decided to evaluate the association between scleral thickness and the latest classifications of central serous chorioretinopathy.
In their paper, published in American Journal of Ophthalmology, the researchers explained that the new categories are further broken down into primary, recurrent and resolved cases, which physicians can then use to determine whether the case is persistent or not. For the study, 167 eyes with simple CSCR and 50 eyes with the complex form were evaluated using OCT.
“The most noteworthy finding was that eyes with complex central serous chorioretinopathy showed significantly thicker sclera than those with simple central serous chorioretinopathy in multivariable logistic regression analysis,” mentioned the researchers in their study. “This result suggested that thick sclera may be involved in an increased area of retinal pigment epithelium atrophy and recurrent and persistent subretinal fluid and may be a poor prognostic factor for central serous chorioretinopathy.” Scleral thickness between complex and simple CSCR in the superior, temporal, inferior and nasal directions were 403.6 vs. 448.4μm, 422 vs. 466.8μm, 439.7μm vs. 482.1μm and 423.6μm vs. 479.2μm. The mean value of scleral thickness in all four directions was 422.2μm ± 44μm vs. 469.1μm ± 44.4μm.
Also, the researchers determined significant predictors of complex CSCR. In their study, they found that older age, male sex, bilateral involvement and the mean value of scleral thickness in all four directions were associated with complex central serous chorioretinopathy. They also discovered that primary CSCR was more commonly associated with simple cases (100 eyes, 59.9% vs. 11 eyes, 22%), while recurrent CSCR was associated with complex ones (62 eyes, 37.1% vs. 39 eyes, 78%).
This study had its limitations. Researchers conducted the work at a single institution, they performed scleral thickness measurements manually and they could not determine the underlying mechanism by which a thick sclera could adversely affect the anatomy in the eye. However, the researchers concluded in their paper that “this study indicated that scleral thickness may play a role in determining the clinical manifestations of central serous chorioretinopathy. A thick sclera could be a risk factor for widespread retinal pigment epithelium atrophy and prolonged subretinal fluid in eyes with central serous chorioretinopathy, which may help devise treatment strategies in clinical practice. Furthermore, new scleral-targeted therapies may be developed for treatment-resistant complex central serous chorioretinopathy.”
Imanaga N, Terao N, Wakugawa S, et al. Scleral thickness in simple versus complex central serous chorioretinopathy. American J Ophthalmol. Jan 22, 2024. [Epub ahead of print]. |

