 |
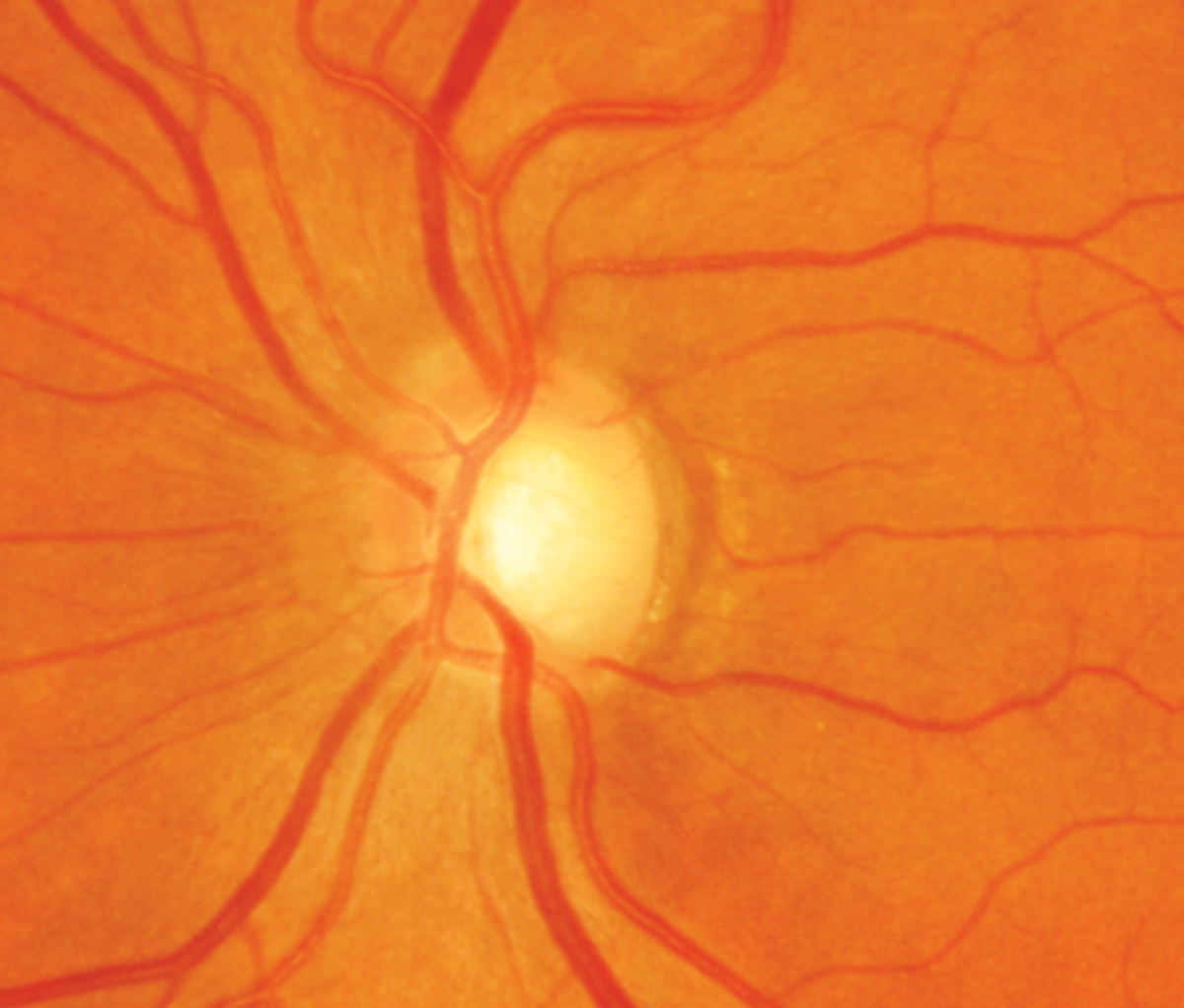
| Roughly 12% of patients in this study with physiologic large cups developed glaucoma during a follow-up of at least 10 years. Photo: Sarah B. Klein, OD. Click image to enlarge. |
Having a large vertical cup/disc ratio has been shown to increase the likelihood of developing glaucoma, though this isn’t the case for all individuals with this anatomic feature. Eyes with a large vertical c/d ratio and no retinal nerve fiber layer defect have what’s referred to as a physiologic large cup (PLC). Because no follow-up guidelines currently exist for these patients, researchers recently performed a study to investigate the natural course of eyes with PLC to identify factors associated with glaucoma development.
The longitudinal study followed 74,572 Korean patients 18 and older for at least 10 and up to 18 years (average: 13.3 years). During this period, the prevalence of PLC among the cohort was 4.78%, and 12.1% of these eyes developed glaucoma after a mean time of 8.7 years (range: 2.0 to 16.5 years). The cumulative incidence of glaucoma conversion was 0.95 cases per 100 person-years.
In patients with large cups, factors appearing to increase the risk of glaucoma conversion included traditional measures like high vertical c/d and violation of the ISNT rule, but also high retinal arterial sclerosis grade and low serum total bilirubin level. Hypertension, heart disease and metabolic syndrome were also more prevalent among the glaucoma conversion group. “The association of serum total bilirubin with glaucoma can be attributed to the antioxidant properties of bilirubin and its role as a biomarker in oxidative stress and inflammation-associated diseases,” the researchers suggested in their paper, published in the American Journal of Ophthalmology.
Interestingly, intraocular pressure (IOP) appeared to have no effect on glaucoma conversion in this population; however, one limitation of the study is that 95% of participants had an IOP measuring between 8.3mm Hg and 19.1mm Hg, which may have led to underestimation of IOP’s effect on disease conversion.
It’s also important to consider that because the study cohort included exclusively patients with Korean ethnicity, the results may not generalize to other populations. Additionally, glaucoma prevalence and conversion rate may have been underestimated, the researchers suggested, since more than half of the cohort was under the age of 50.
Based on the data, the researchers concluded in their paper, published in the American Journal of Ophthalmology, that, “Considering the relatively low glaucoma conversion rate for PLC, a comprehensive glaucoma examination every year may not be necessary for all PLC subjects.” They suggested instead that “clinicians can identify and concentrate on subjects at relatively high risk of developing glaucoma and who are more likely to benefit from a customized surveillance program.”
Choe S, Kim YK, Park KH, Choi HJ, Jeoung JW. Natural history of optic disc with physiologic large cup: incidence, predictors of glaucoma conversion after minimum-10-year follow-up. Am J Ophthalmol. July 2, 2023. [Epub ahead of print]. |

