High altitude can pose several challenges for individuals who live in such environments permanently or long-term, as the human body undergoes physiological changes that include increased heart rate, hyperventilation and alterations in hematological features. These effects overlap with the mechanisms seen in various chronic metabolic diseases, such as diabetes mellitus. Since diabetic retinopathy (DR) risk is an obvious concern in these individuals and is one of the leading causes of blindness, Chinese researchers with backgrounds in genetics and ophthalmology considered the effect of high altitude on DR in a recent literature review.
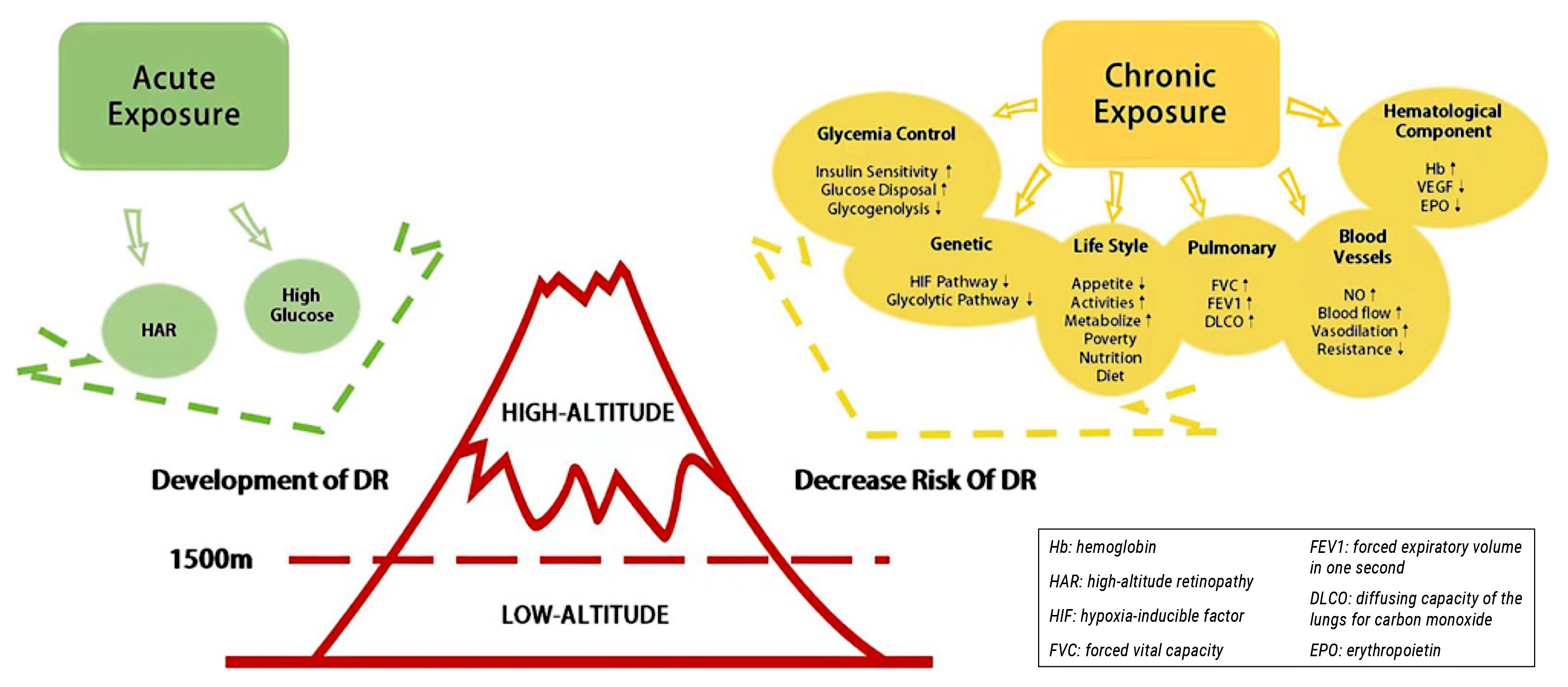 |
| The high-altitude hypoxic environment in high-altitude areas activates transient hyperglycemia and increases the risk of diabetic microangiopathy and high-altitude retinopathy, which may alleviate the progression of diabetic retinopathy. Photo: Gong H. Ophthalm Res. Dec. 16, 2023. Click image to enlarge. |
Exposure to high altitude “triggers complex adaptive mechanisms to protect the internal homeostasis of the human body under hypoxia and low air pressure,” they stated in their paper. They elaborated that effects differ based on duration of exposure (short- vs. long-term) as well as numerous confounding influences, including genetic backgrounds, living conditions and dietary habits.
Enhanced dense capillaries and vasodilation adaptation not only increase oxygen delivery in highlanders with diabetes, they speculated, but also might mitigate microvascular complications such as DR. “However,” they countered, “for those acutely exposed to high-altitude areas, the high-altitude hypoxic environment significantly activates transient hyperglycemia and increases the risk of diabetic microangiopathy and high-altitude retinopathy.”
Also, a previous study showed that hyperglycemia-induced retinal damage includes the polyol pathway, advanced glycation end-product accumulation, the protein kinase C pathway and the hexosamine pathway. “Therefore, there is no doubt that improved glycemic control and lower blood glucose might reduce the risk of DR caused by hyperglycemia in diabetes mellitus patients,” the authors suggested.
In conclusion, for those acutely exposed to high-altitude areas, the high-altitude hypoxic environment significantly activates transient hyperglycemia and increases the risk of diabetic microangiopathy and high-altitude retinopathy.
“Residents in high-altitude areas are less likely to suffer from diabetic microangiopathy due to factors such as improved glucose control, lifestyle and nutrition selection, genetic adaptation, stronger lung function, increased blood vessel vasodilation, higher serum Hb concentration, lower VEGF levels and a blunted erythropoietin response,” the authors explained. “However, there are limited studies designed to point out the reverse risk of altitude and complications of diabetes in participants with specific characteristics (e.g., type and duration of diabetes, altitude, age and sex).
“Future clinical research should include a diverse group of participants to confirm the potential beneficial influence of high altitude on DR,” the authors advocated. “This would enhance our understanding of the intriguing relationship between altitude and DR and potentially lead to the exploration of new therapeutics for DR.”
Gong H, Zhou Q, Gama Z, Lan Y. High altitude exposure and diabetic retinopathy: unveiling the impact and mechanisms of alleviation. Ophthalm Res. Dec. 16, 2023. [Epub ahead of print.] |

