 |
|
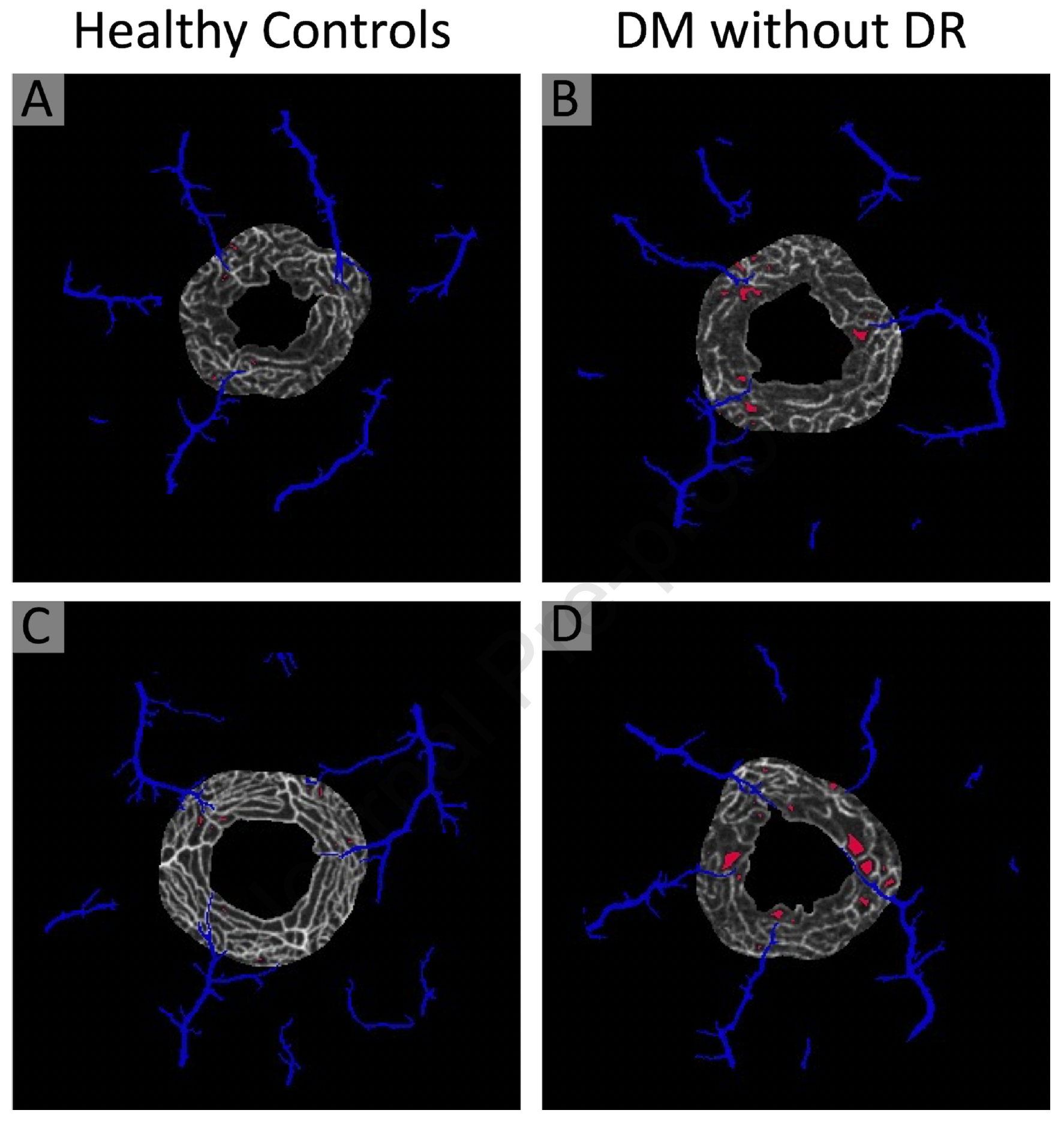
OCT angiography of patients with diabetes without diabetic retinopathy showed macular perfusion deficits were significantly increased in the perivenular deep capillaries (shown in red) compared to healthy controls. Photo: Nesper PL, et al. Ophthalmol Sci. Jan 26, 2024. Click image to enlarge. |
Microvascular alterations are a central feature of diabetic retinopathy (DR), a leading cause of visual impairment, and retinal imaging has played an important role in identifying early vascular changes even before disease onset. As such, OCT angiography (OCT-A) has been beneficial for studying capillary changes that occur in patients with diabetes mellitus (DM) without diabetic retinopathy (DR). A new study published in Ophthalmology Science identified significant perfusion deficits in the perivenular deep capillaries near the fovea in these patients using OCTA, suggesting this area may be more susceptible to vascular injury and disruption during diabetes.
The retrospective, cross-sectional study included 16 eyes of healthy subjects and 16 eyes of those with DM without DR, all of whom underwent repeated 3 x 3 mm OCT-A macular scans centered at the fovea during a single session. Geometric perfusion deficit measurements were significantly increased in the 300μm surrounding the foveal avascular zone in the full retina, superficial capillary plexus and deep capillary plexus. Further inspection revealed that only the 100 μm perivenular region in the deep capillary plexus had significantly increased perfusion deficits, suggesting this region nearest the foveal avascular zone is particularly susceptible to early capillary closure and flow abnormalities in DM.
The study authors say these findings corroborate earlier reports showing deep capillary alterations are associated with decreased central visual function in patients with DM without retinopathy. It also suggests the 300μm surrounding the foveal avascular zone may be the most important area of capillary change. “By partitioning this ‘FD300’ region into perivenular, periarteriolar and capillary zones, we were able to distinguish the central perivenular deep capillary zone as the most significant biomarker for distinguishing patients with DM without DR,” the authors stated. “It is worth highlighting that this 300μm ring is also the region with the greatest density of cone photoreceptors. Therefore, this foveal region of perivenular deep capillaries may be particularly susceptible to vascular damage.”
Larger studies are needed to confirm and support these results, continued the authors. “Limitations of this study include a small number of eyes due to our strict inclusion and quality criteria,” they said. “We were limited to the DM without DR group and future studies expanding this methodology would help elucidate the progression of capillary abnormalities throughout the stages of DR. We also acknowledge the inherent limitations of OCT-A technology, which may potentially limit complete visualization of the deep retinal vasculature. Finally, we only assessed the macula, but future studies using faster scanning and wider field OCT-A could provide high-quality macular and peripheral vasculature assessment.”
However, this study bolsters previous hypotheses regarding early pathological biomarkers in preclinical DR, therefore identifying the central perivenular deep capillaries as prime targets for further analysis.
Nesper PL, Fawzi AA. Perfusion deficits in diabetes without retinopathy localize to the perivenular deep capillaries near the fovea on OCT Angiography. Ophthalmol Sci. January 26, 2024. [Epub ahead of print]. |

