 |
A 65-year-old Hispanic female was referred by her ophthalmologist for evaluation of decreased vision in her left eye. Her symptoms consisted of blurry vision and metamorphopsia in the left eye for the past 10 months.
Her medical history was significant for hypertension, arthritis, high cholesterol, heart disease and non-insulin dependent diabetes mellitus. Her last glycosylated hemoglobin (HbA1C) was 6.1%.
The referring doctor had administered an injection in the left eye to improve her vision, but the patient said it did not help.
Best-corrected visual acuity at this visit was 20/20 O.D. and 20/40 O.S. Confrontation fields were full to finger counting O.U. Amsler grid was normal in the right eye, but revealed metamorphopsia paracentrally O.S. Extraocular motility was full, and the patient denied pain or diplopia. Pupils were round and briskly reactive to light without afferent pupillary defect. IOP measured 16mm Hg O.U. Anterior segment exam was remarkable for 1+ nuclear sclerosis of both lenses.
 |
 |
|
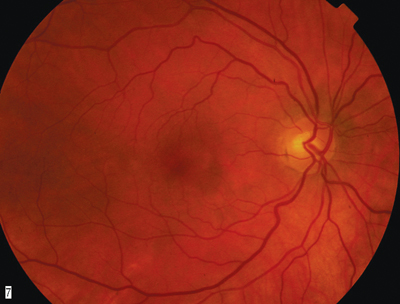
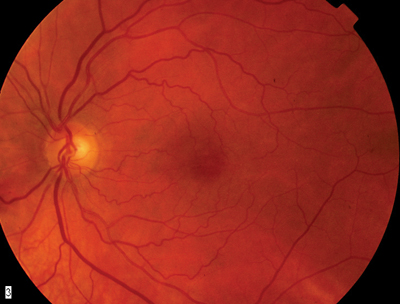
1, 2. Fundus photos (O.D. left, O.S. right) show subtle changes in the macular region. |
 |
|
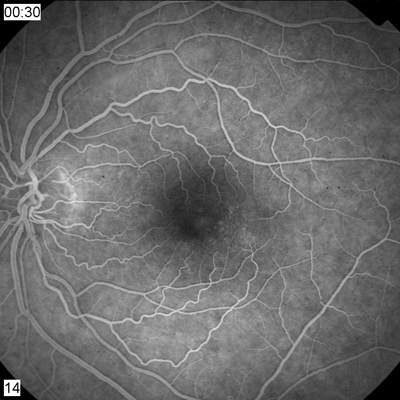
3. Fluorescein angiogram of the left eye shows an abnormal leakage pattern. |
 |
|
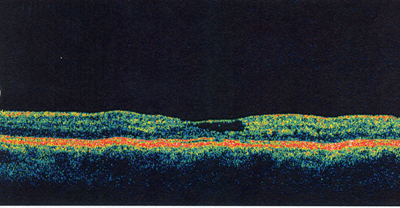
4. OCT reveals a thin layer that crosses over a cystoid space in the fovea O.S. |
1. What do the findings on the fluorescein angiogram represent?
a. Microaneurysms.
b. Retinal telangiectasis.
c. Cystoid macular edema.
d. Intraretinal neovascularization.
2. What is the best interpretation of the OCT?
a. Internal limiting membrane drape.
b. Cystoid macular edema.
c. Intraretinal neovascularization.
d. Diabetic macular edema.
3. What is the likely diagnosis?
a. Nonproliferative diabetic retinopathy.
b. Hypertensive retinopathy.
c. Idiopathic juxtafoveal retinal telangiectasis.
d. Diabetic macular edema.
4. The best treatment option for patients who have this condition is:
a. Photodynamic therapy (PDT).
b. Intravitreal Kenalog (triamcinolone acetonide) injection.
c. Focal grid laser.
d. Observation.
5. What treatment did the referring physician give the patient?
a. Intravitreal Kenalog.
b. Intravitreal Avastin.
c. Sub-Tenons steroid injection.
d. Juxtaslceral Kenalog injection.
For answers, go to bottom of page.
Discussion
The right fundus appears normal except for two microaneurysms in the temporal aspect of the macular region. A small area of seemingly abnormal retinal vessels, microaneurysms and retinal thickening appears temporal to the fovea O.S.
Fluorescein angiography shows early hyperfluorescence in the area corresponding to these changes. In later frames in both eyes, there is leakage of fluorescein in the area temporal to the fovea.
The abnormal vessels represent dilated telangiectatic vessels. While they are more prominent O.S., the angiogram shows that they are also present O.D.
In 1982, J. Donald M. Gass and R.T. Oyakawa described a disease associated with incompetent, telangiectatic capillaries localized solely to the juxtafoveal or perifoveal area of the retina.1 They developed a classification and staging of the disease entity we now know as idiopathic juxtafoveal retinal telangiectasis (IJRT). Dr. Gass classified the disease as follows:1
Group 1A: unilateral, congenital juxtafoveal telangiectasis of retinal capillaries temporal to the fovea.
Group 1B: idiopathic, unilateral telangiectasis with an area of focal capillary incompetence adjacent to the foveal avascular zone.
Group 2A: idiopathic, bilateral, acquired juxtafoveal retinal telangiectasis.
Group 2B: occult, familial juxtafoveal telangiectasis.
Group 3A: idiopathic, occlusive juxtafoveal telangiectasis.
Group 3B: idiopathic, occlusive juxtafoveal telangiectasis associated with central nervous system vascular abnormalities.
Groups 1B and 2A are the most common forms O.D.s encounter in clinical practice.2 Group 1B is more commonly seen in men past age 40 and likely represents a spectrum of Coats disease. Group 2A is seen in men and women alike and typically presents between ages 40 and 60. Based on the clinical findings, angiogram and bilaterality, we diagnosed our patient with Group 2A IJRT.
Group 2A typically presents with bilateral thickening of the temporal region of the fovea and right angle venules, which appear as vessels that dive down at right angles into the retina. Patients with Group 2A IJRT exhibit minimal serous exudation, no lipid exudation into the retina and, later in the disease, retinal pigment epithelial hyperplastic plaques and crystalline deposits. A subretinal neovascular membrane, which sometimes develops, is the most visually compromising manifestation of IJRT.
Right angle venules, RPE plaques and neovascular membranes may represent chorioretinal anastamoses and may be indicative of severe, focal vascular incompetence and ischemia.2 Chorioretinal anastamoses may precede severe and rapid vision loss in these patients.
OCT of our patients left eye shows an internal limiting membrane (ILM) drape, which is pathopneumonic for IJRT. This drape is a thin layer that crosses over a cystoid space in the fovea. It represents an area of focal loss of the outer plexiform layer secondary to a cystoid space in the center of the fovea.
The ILM drape seen in IJRT is unique in that there is normal retinal contour and thickness in the surrounding retina. There is no adjacent edema, and there are no cystic spaces in the area immediately surrounding the central fovea.3 The ILM drape is more commonly seen in Group 2A and is believed to be exclusive to this variant.
The visual prognosis of patients with Group 2A IJRT is not good. It seems to be a progressive condition; vision loss secondary to neovascular membranes often is the final course.
Currently, there is no effective treatment for IJRT. Observation tends to be the norm. However, in cases in which neovascular membranes develop, treatments such as PDT and intravitreal anti-VEGF (vascular endothelial growth factor) injections are being investigated.
PDT shows promise for treating subretinal neovascularization secondary to Group 2A IJRT.2 While the neovascularization seems to originate in the retina instead of the choroid, studies show at least maintenance of baseline visual acuity in most patients treated with PDT.
Anti-VEGF drugs, such as Avastin (bevacizumab, Genentech), have been used to treat the macular edema and may offer the best hope for treating this condition. This is currently being investigated.
Our patient is stable with visual acuity of 20/20 O.D. and 20/40 O.S. We gave her a new spectacle Rx, educated her about her condition, and gave her an Amsler grid with instructions to return if she noted any changes. We follow her every three to four months with fundus photos, fluorescein angiography and OCT.
This case was co-written by Noemi Zubizarreta, O.D., an optometric resident at Bascom Palmer Eye Institute in Miami.
1. Gass JD, Oyakawa RT. Idiopathic juxtafoveal retinal telangiectasis. Arch Ophthalmol 1982 May;100(5):769-80.
2. Snyers B, Verougstraete C, Postelmans L, et al. Photodynamic therapy of subfoveal neovascular membranes in type 2A idiopathic juxtafoveolar retinal telangiectasis. Am J Ophthalmol 2004 May;137(5):812-9.
3. Paunescu LA, Ko TH, Duker JS, et al. Idiopathic juxtafoveal retinal telangiectasis: new findings by ultrahigh-resolution optical coherence tomography. Ophthalmology 2006 Jan;113(1):48-57.
Answers: 1) b; 2) a; 3) c; 4) d; 5) a.

