 |
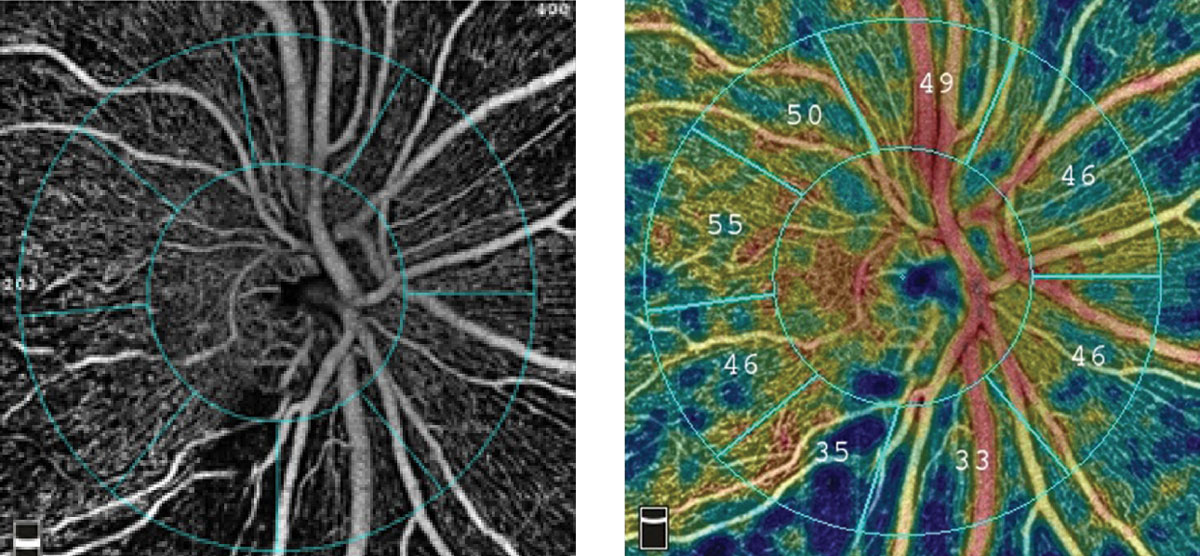
| This study demonstrated that the PACG eye had significantly lower vascular perfusion than the control group in every sector of the optic area and macular area (except the nasal sector of parafoveal). Photo: Optovue. Click image to enlarge. |
There has been an increase in interest in the vascular components of glaucoma in recent years. OCT-A is a novel and noninvasive blood flow imaging technique, which can not only provide structure information but also quantitatively measure the retina and choroid perfusion. Researchers based in China evaluated the diagnostic ability of the papillary and macular vessel density in different sectors and layers on OCT-A in primary angle closure glaucoma (PACG) and acute primary angle closure, and to compare these with peripapillary RNFL thickness and ganglion cell complex (GCC) thickness measured by spectral-domain OCT. The study found that, whatever IOP increased slowly or rapidly, the optic disc area vascular perfusion was more valuable for the diagnosis of glaucoma compared with the macular area.
The cross-sectional, observational study included 22 acute primary angle closure patients (22 eyes) and 21 primary angle closure patients (27 eyes) along with 17 healthy people. Optic disc region and macular region were imaged using swept-source OCT-A, while circumpapillary retinal nerve fiber layer (cpRNFL) thickness and GCC thickness were obtained by spectral-domain OCT.
Compared with the healthy group, the cpRNFL thickness in the superior sector was thicker in the acute primary angle closure group, and this area had the most diffuse microvascular dropout as well. The difference in the macular superficial capillary plexus vessel density between the acute primary angle closure and the control groups was not statistically significant. The area under the curve of the total optic disc vessel density in the radial peripapillary capillary layer was higher than the area under the curve of the papillary vessel density in the optic nerve head (ONH) layer.
Compared with the control group, the total optic disc vessel density, peripapillary vessel density and each quadrant of peripapillary vessel density were decreased in PACG. In this group, the macular region, SCP vessel density, deep capillary plexus vessel density and parafovea vessel density (except temporal sectors) decreased. The PACG eyes had a greater decrease of vessel density in total ONH than total macula. The diagnostic value of the vessel density in the ONH layer and the radial peripapillary capillary layer was similar. The diagnostic value of the superficial capillary plexus vessel density in the macula was greater than the deep capillary plexus vessel density in the macula.
“Radial peripapillary capillary and ONH papillary vessel density, macular superficial vessel density detected glaucoma with high accuracy and could be valuable in the diagnosis of glaucoma,” the researchers wrote in their paper. “The radial peripapillary capillary layer exists in the superficial layer around the optic disc and is proportional to the thickness of RNFL; this layer may be the main vascular network that nourishes the RNFL.”
The study concluded that, “the OCT-A vascular parameters have similar performance to the OCT structural parameters for glaucoma diagnosis in primary angle closure glaucoma.”
Li C, Tan L, Xu X, Chen S, Huang C. Changes of optic disc and macular vessel perfusion density in primary angle closure glaucoma: a quantitative study using optical coherence tomography angiograph. Ophthalmic Res. August 30, 2023. [Epub ahead of print]. |

