Practical Matters in Myopia ManagementWith an expanding arsenal of information, myopia can be a puzzling area of care. In this second annual Review of Optometry supplement, experts offer solutions backed by science to help you manage this growing patient population. Click here to download a PDF. Check out the other articles featured in this supplement: |
As eyecare professionals, we have many opportunities each day to positively impact our patients’ lives and eye health. Myopia management presents as certainly one of those opportunities—simple recommendations and strategic interventions can alter the entire trajectory of a patient’s prescription that will ultimately decrease their risk for eye disease and improve their quality of life.
Who is a good candidate for myopia management?
When assessing a prospective candidate, bear in mind that previous myopia progression is not necessarily predictive of future progression. This statement works both ways—current prescription or axial length stability does not guarantee future stability and current progression does not predict future progression. Unfortunately, there is no reliable method to determine which category a particular child will fall in. Thus, clinicians should also consider a series of risk factors such as age of myopia onset, ethnicity, parental myopia, lifestyle, outdoor time, amount of near work and axial length.
With these thoughts in mind, deciding when to initiate myopia management can be tailored to each patient. Since myopia is progressive in the vast majority of children in which it manifests, adopting the mindset that all myopes beginning with refractions of -0.50D will benefit from myopia management is absolutely warranted. The commonly used phrase “every diopter matters” stems from the fact that slowing myopia progression by 1.00D reduces a patient’s risk of developing myopic maculopathy, the most serious and sight-threatening consequence of myopia, by 40% regardless of the level of myopia.1
How do I discuss the benefits of myopia management with parents?
In most cases, parents are highly intrigued by the notion of controlling their child’s myopia, especially if one or both parents experienced progressive myopia as a child. First off, they will likely want to know how their child became myopic or why their child’s prescription is on track to surpass their own. Start the discussion with the fact that the world looks different than it did a few decades ago—kids now spend significantly less time outdoors and more time indoors on digital devices both at home and in school. This indoor/outdoor imbalance appears to be an uncontrollable variable and is contributing to a myopia epidemic worldwide.
We as a profession have adapted and shifted our focus—we no longer have to helplessly watch a child’s prescription creep up; instead, we recommend myopia management. In fact, the World Council of Optometry in 2021 declared myopia management to be the standard of care. Fortunately, we now have several safe and effective options to help us accomplish the goal of myopia management, one of which is FDA approved. Secondly, be sure to clearly define success. Myopia management does not equate to preventing myopia progression or axial elongation but instead slowing it down. Conveying this distinction is imperative. The most widely accepted metric for success is slowing myopia progression by at least 50%.
 |
|
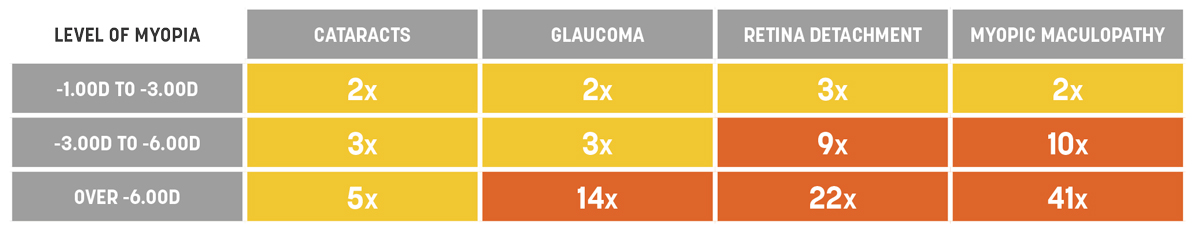
Fig. 1. Odds ratios of increased risk of ocular pathology with increasing levels of myopia.2 Click image to enlarge. |
To put this into perspective for parents, give them an example. Their child’s prescription increased by 1.00D this past year, but had they been using some form of myopia control for that year, we would, ideally, expect only 0.50D of progression or less. Lastly, we must gently impress upon parents that myopia is not just being nearsighted, but it is, more importantly, elongation of the eye beyond what is normal for their child’s age. This axial length elongation puts their child at increased risk for pathologies like primary open-angle glaucoma, cataracts, retinal detachment and myopic maculopathy (Figure 1).2 The goal of this part of the conversation is not to instill fear in the parents but to give concrete value to what we are trying to accomplish with myopia management. In addition, this reiterates that simply updating their child’s glasses or contact lens prescription is not the appropriate solution. Drive home the idea that the goal for myopia control is a 50% reduction in progression. Many parents don’t understand what that means.
After diving into these few points, most parents appreciate the expertise and willingness to help their child. The bottom line is that parents want what’s best for their children and, at the very least, they want as much information as their eyecare provider can offer. Even if they do not sign up for a myopia management program at the first visit, by starting the conversation the practitioner has fulfilled their obligation with educating the family.
 |
|
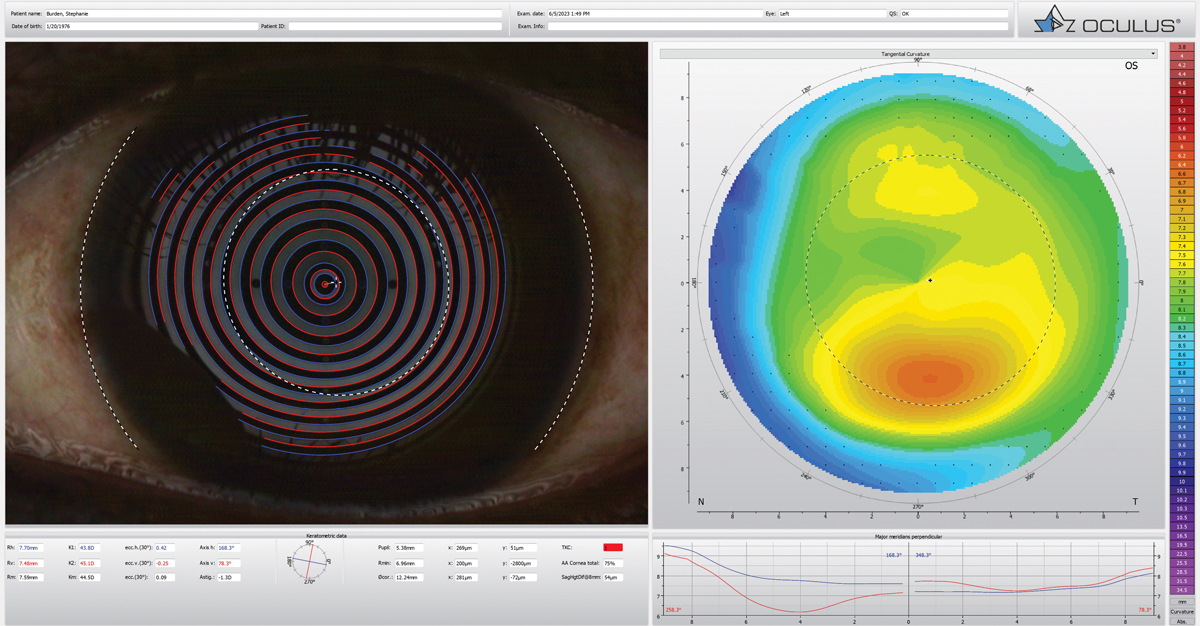
Fig. 2. Corneal topography can be a huge help in a myopia control practice. Click image to enlarge. |
We have decided to proceed with myopia management—now what?
Prior to starting a myopia management modality of any kind, a thorough, comprehensive baseline examination should be completed. This is good clinical practice but also provides valuable baseline data that will be used to measure success. This exam includes:
Binocular vision assessment. Because myopia management strategies may impact binocular vision function and vice versa, a binocular vision assessment can provide helpful information on which treatment to choose. Specific tests recommended by the International Myopia Institute include distance and near cover test, near point of convergence, amplitude of accommodation, distance and near accommodative facility, accommodative accuracy (lead/lag), accommodative convergence/accommodation (AC/A) ratio and near fixation disparity (MEM).3 Any binocular vision disorder, especially if symptomatic, should be managed before the commencement of myopia control efforts. Improved binocular vision function will also, ultimately, improve the patient’s success in myopia management.
Cycloplegic refraction. The key to an accurate refraction in children is controlling accommodation. This is most commonly achieved with two drops of cyclopentolate 1% given five minutes apart, followed by a waiting period of 30 to 45 minutes. If the child is cooperative, cycloplegic autorefraction provides an excellent starting point for refraction. Oftentimes in younger children, a standard or handheld auto-refraction is the only measure of refractive error that can be obtained until the child is mature enough to provide reliable answers during refraction.
Anterior segment assessment. A thorough slit-lamp examination is necessary, especially for a patient who will potentially be wearing contact lenses of any kind. Give special attention to signs of dry eye and/or meibomian gland dysfunction. If noted, these should be treated before a contact lens fitting.
Topography. In order to truly determine if a patient is an adequate orthokeratology (ortho-K) candidate, corneal topography is warranted (Figure 2). Be sure to rule out keratoconus or any other corneal irregularity that would contraindicate ortho-K.
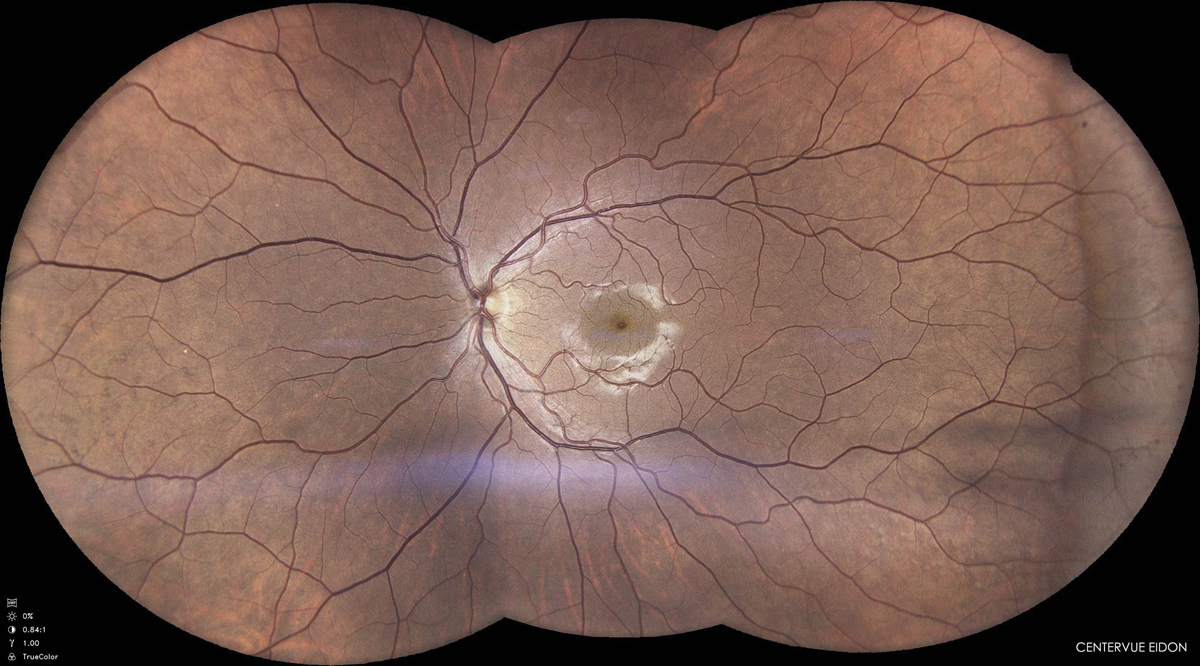
Dilated fundus examination. Assess the retina for any current myopic changes and set a baseline for future comparisons. Fundus photography is an excellent adjunct to a dilated fundus exam and can be a great visual for both parents and the patient (Figure 3).
Axial length. Although measuring axial length has yet to be widely adopted into everyday practice, its acceptance and value in myopia management is rapidly growing. Currently, there are several ultrasound devices and optical biometers on the market. Perhaps the most cost-effective options, however, are combination devices that not only measure axial length but also provide a plethora of additional information like topography, pupillometry and progression maps.
Obtaining a child’s baseline axial length allows the practitioner to compare it with a normative chart and, thus, assess their risk for future progression. Consider sharing your assessment with the parents—they typically equate this information to height and weight measurement at the pediatrician. Simply knowing the value puts their child’s current status into perspective. This is also another educational opportunity to reiterate that the goal of myopia management is to slow elongation of the eye which, in turn, slows myopia progression.
Pupil assessment. This responsibility is the same as in any routine exam—measure and record the size in both dim and bright illumination, check for an afferent pupillary defect and any other pupil anomaly. If any pupil abnormality is present, further investigation is warranted and use of a pharmaceutical agent for myopia control would be contraindicated.
Gathering baseline pupil measurements serves two additional purposes. If topical low-dose therapy is chosen, the practitioner can determine if there is a significant dilation effect that could be bothersome to the patient. Larger pupils may also be a contraindication for ortho-K due to the potential impact of visual disturbances like halo and glare in low-light situations.4
 |
|
Fig. 3. Assess the retina with a dilated fundus examination for any current myopic changes and set a baseline for future comparisons. Click image to enlarge. |
How do I choose which myopia management option is best?
Currently, the three most wildly available forms of myopia control are pharmaceutical therapy with low-dose atropine, soft multifocal or dual focus lenses, and ortho-K. Although each of these strategies could be successful for any given patient, there are special considerations for each. Atropine may be best reserved for younger patients who are not yet mature enough for contact lenses or for those who are unable or unwilling to wear contact lenses. Soft contact lenses are an excellent option for children who are current soft lens wearers and for patients mature enough to handle potential daytime nuances of soft contact lens wear (Figure 4). Lastly, ortho-K is the best option for any patient wishing to have freedom from daytime contact lens wear or for younger patients whose parents wish to maintain control of contact lens wear within the household.
 |
|
Fig. 4. Consider whether patients are mature enough to be responsible with soft contact lenses. Click image to enlarge. |
It is important to note that there is currently only one FDA-approved option for myopia control—CooperVision’s MiSight 1-day lens. Although the other options are not approved by the FDA for myopia control, many studies support their use for such purposes and validate their efficacy. For complete transparency, this information about FDA approval should be included in the discussion about which option is best suited for a child as this may impact a family’s decision.
In addition, there are simple lifestyle changes that can enhance any of the above modalities, whether it be the treatment of choice for parents not ready to start a more traditional modality or a strategy to prevent myopia in pre-myopic children. Spending more time outdoors is the most common recommendation and has been recognized for years to prevent or delay myopia onset. The current recommendation is now is to spend at least two hours per day outdoors, but the more time the better; in fact, children who spent less than 13 hours per week outdoors have a significantly higher risk of incident myopia.5 Limiting near work to 30 continuous minutes or less and increasing the near working distance to at least 30cm are also useful recommendations.6
When do I follow-up?
Ongoing care for each treatment modality is slightly different and can vary depending on the needs of the patient and the clinician’s comfort level. Below is a recommended follow-up schedule for each myopia management modality.
At the six-month follow-up, regardless of modality, repeat the cycloplegic refraction and axial length measurements. All additional baseline testing should be completed annually.
Atropine: One week after start, then quarterly.
At each visit, assess pupil size to ensure the dilation effect is stable from visit to visit. Also, ask the patient if they are experiencing an uncomfortable amount of photosensitivity, near blur or any other ocular or systemic side effects. If so, consider reducing the dose first before discontinuing altogether. Note, according to the Low-Dose Atropine for Myopia Progression (LAMP) trial, the recommended starting dose for atropine is 0.05%, but lower doses of 0.025% and 0.01%, although less effective, are also in use.7 The key is to find a dosage for the patient that is tolerable and provides adequate myopia control.
Soft contact lenses: One week after start, then quarterly.
Once a patient is well-established in soft lenses, the practitioner should routinely assess the fit of the lens and the patient’s ocular health. A spherical overrefraction with loose lenses provides a quick assessment of potential refractive error change. However, the most accurate assessment is the cycloplegic refraction done biannually.
Ortho-K: One day after start; one week after start; one month after, then quarterly.
Orthokeratology follow-ups can be the most variable because they depend on how well the initial lens design fits the patient. The above schedule is for the ideal lens design. More frequent follow-ups will be warranted if changes to the lens design are made at any point during the fitting process. At each visit, topography is warranted to determine proper centration and treatment of the lens. A refraction, whether cycloplegic or not, usually doesn’t provide the most helpful information since the goal of ortho-K is to eliminate refractive error. For these patients, axial length is the best measure of refractive change which should be performed biannually along with the cycloplegic refraction.
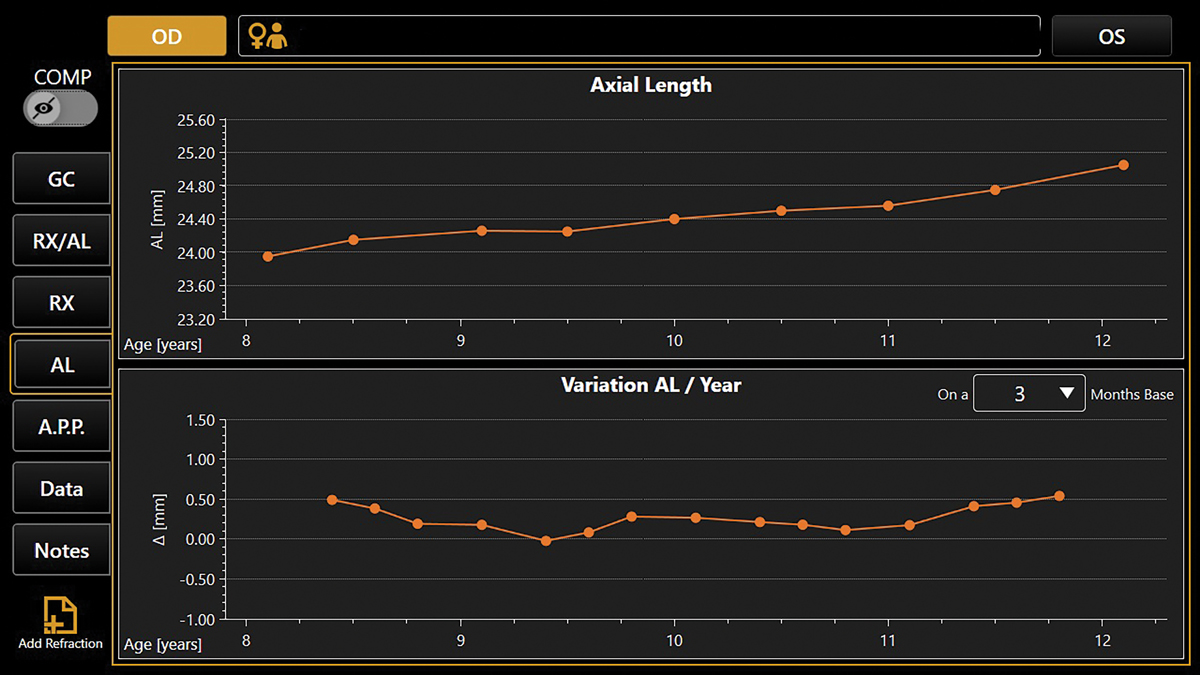 |
| Fig. 5. Progression maps on combination devices can provide an excellent visual on the effect of myopia management for both the practitioner and parent. Click image to enlarge. |
How is success defined?
As mentioned above, most practitioners agree that a myopia management modality is considered successful if myopic progression has been slowed by at least 50%. Since no one can predict the future, it is impossible to know whether we have achieved this goal from year to year. However, the best predictor of the future is the past. Thus, if the child progressed—in refractive error and/or axial length—no more than half of what they had progressed in the year prior, then the clinician can consider their efforts successful. When assessing myopia control success in terms of axial length, the general goal is to achieve <0.2mm elongation in children under 10 years old and <0.1mm elongation in children over 10 years old per year.8,9
Since we have such effective myopia management options available to us now, there will be some children who hardly progress or do not progress at all. For those who do progress, be sure to put the progression into perspective and focus on the fact that had no myopia management been put into place, there would certainly be more significant progression. In addition, if the amount of progression slowing does not meet or exceeds your expectations, then switching to a different modality or combination therapy may need to be considered.
Combination therapy for myopia most commonly includes coupling low-dose atropine with soft contact lenses or ortho-K. This would also be an appropriate time to review with patients and parents the importance of outdoor time and near work habits.
A major advantage of the combination devices mentioned earlier is the built-in progression maps that some of these devices offer (Figure 5). They can plot both refractive error and axial length for each visit, which provides an excellent visual for both the practitioner and parents. Both stability and instability can be easily visualized, making the conversation on whether success is being achieved much easier.
How long should a patient continue myopia management?
There is no consensus amongst practitioners on exactly what age or how many years a patient should partake in myopia management, simply because every patient is different and unpredictable. We know that myopia progression is fastest in younger patients and tends to slow down during the teenage years. Thus, parents may want to discontinue myopia management once their teenager has shown consecutive years of stability. On the other hand, it is also reasonable to continue indefinitely, especially if the patient is a contact lens wearer and is happy with comfort and vision. Keep in mind that the COMET study found that at age 15, 50% of myopes were still progressing.10 This may be useful information when parents are indecisive. Atropine as a monotherapy, however, is typically only used until the child can transition into a contact lens option, but there is no solid evidence that children cannot use atropine long term. As with use of any pharmaceutical, practitioners should routinely follow-up with the patient and adjust the treatment plan if needed.
Takeaways
Myopia management is life-changing and is truly a gift that should be offered to every child in your practice. Whether it is lifestyle recommendations, contact lenses or atropine, a child will benefit from any intervention set into place. It starts with effective communication and education that may need to occur several times before the parents say “Yes.” Remember: Every single child deserves the opportunity to have better vision and quality of life; it is our job to make it happen.
1. Bullimore MA, Brennan NA. Myopia control: why each diopter matters. Optom Vis Sci. 2019;96(6):463-5. 2. Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012;31(6):622-60. 3. Gifford KL, Richdale K, Kang P, et al. IMI—clinical management guidelines report. Invest Ophthalmol Vis Sci. 2019;60:M184-203. 4. Takahiro H, Chikako O, Yuko I, et al. Contrast sensitivity function and ocular higher-order aberrations following overnight orthokeratology. Invest Ophthalmol Vis Sci. 2007;48(2):550-6. 5. Xiong S, Sankaridurg P, Naduvilath T, et al. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmol. 2017;95(6):551-66. 6. Huang PC, Hsiao YC, Tsai CY, et al. Protective behaviours of near work and time outdoors in myopia prevalence and progression in myopic children: a two-year prospective population study. Br J Ophthalmol. 2020;104(7):956-61. 7. Yam JC, Li FF, Zhang X, et al. Two-year clinical trial of the Low-Concentration Atropine for Myopia Progression (LAMP) Study: Phase II Report. Ophthalmology. 2020;127(7):910-9. 8. Mutti DO, Hayes JR, Mitchell GL et al. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Invest Ophthalmol Vis Sci. 2007;48(6):2510-9. 9. Tideman JWL, Polling JR, Vingerling JR, et al. Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol. 2018;96(3):301-9. 10. COMET Group. Myopia stabilization and associated factors among participants in the Correction of Myopia Evaluation Trial (COMET). Invest Ophthalmol Vis Sci. 2013;54(13):7871-84. |

