 |
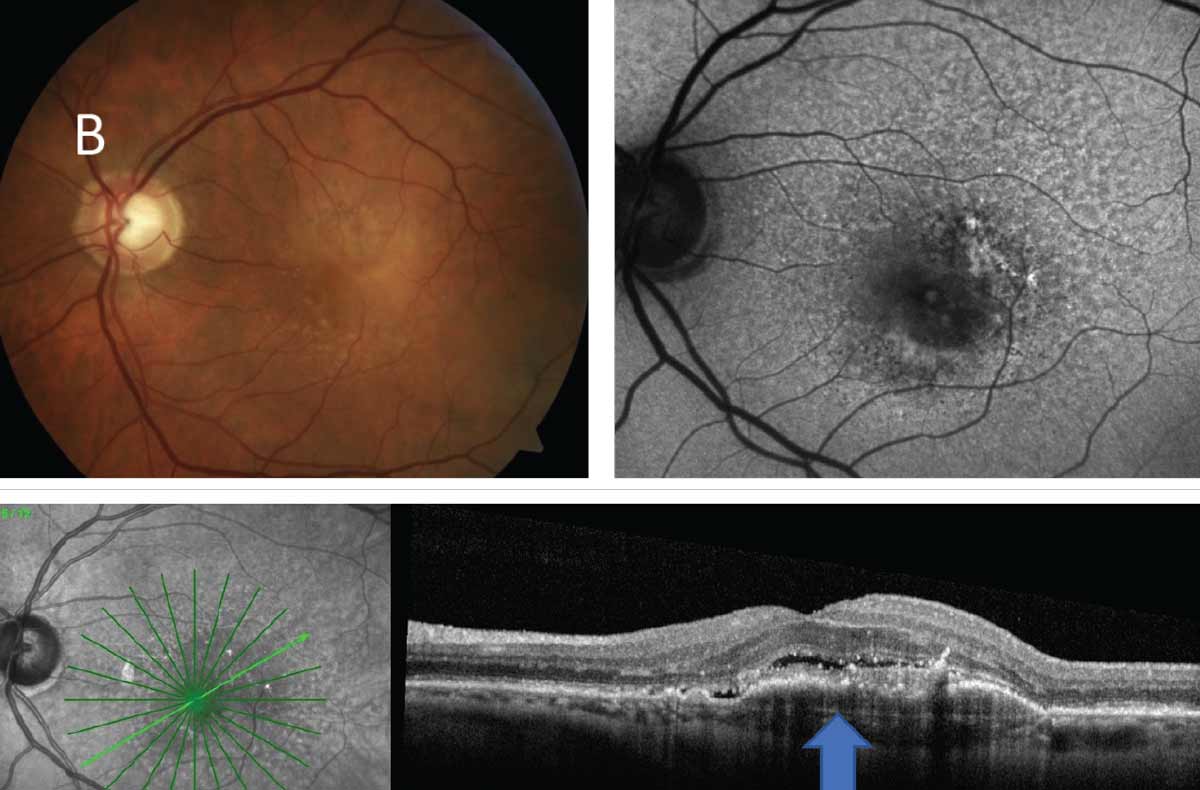
End-stage nAMD patients shouldn’t be subjected to continued intravitreal injections, researchers argue. Photo: Mohammad Rafieetary, OD. Click image to enlarge. |
In a new study, researchers reported the functional and anatomical outcomes of intentionally suspending anti-VEGF injections in 93 eyes with advanced neovascular age-related macular degeneration (nAMD). They found that stopping anti-VEGF treatment is acceptable in advanced nAMD (VA≤20/400) patients when there’s a high rate of lesion stability.
There was no significant change in central foveal thickness (CFT) or lesion size up to two years following the stoppage of treatment, but there was a progressive decrease in the prevalence of IRF at the six-, 12-, 18- and 24-month follow-up visits. VA remained stable at 24 months after treatment suspension except for a slight decrease at six and 12 months.
One explanation for the acceptable stoppage of treatment is the eventual stability of end-stage lesions. “The natural history of nAMD suggests that lesions at the disciform scarring stage tend to stabilize even without treatment,” the authors explained in the study.
“While we observed a small decrease in VA at six and 12 months after treatment suspension, it is likely not clinically significant and may represent fluctuations related to the advanced disease as well as non-standardized office-based VA testing that may be even less reliable given the poorer levels of vision,” the authors continued. “Given the imprecise nature of VA measurements in advanced nAMD, which can fluctuate considerably between visits depending on provider technique, the stable OCT parameters and reduction in IRF are reassuring indicators that treatment suspension was likely not detrimental.”
Another reason is there is a lower risk of clinically significant vision loss.
“Although experts have rightly cautioned against treatment suspension due to a risk of irreversible vision loss following CNV reactivation, it is essential to distinguish eyes with end-stage disease and low VA,” the authors noted in the study. “We chose 20/400 as the cutoff in part because most of the phase III pivotal clinical trials on anti-VEGF therapy excluded eyes with VA worse than 20/200, so there is little good data on patients with poorer vision. Moreover, while most would consider 20/400 as being poor vision from a functional standpoint, the majority of our patients were CF or worse.”
Overall, the incidence of restarting treatment was 2.2% of eyes after 24 months and 5.4% of additional eyes by the final visit, with recurrent CNV activity cited as the most common reason.
Awh KC, Mahoudzadeh R, Salabati M, et al. Outcomes of intentionally suspending treatment in eyes with advanced neovascular age-related degeneration. Am J Ophthalmol. July 24, 2023. [Epub ahead of print.] |

