 |
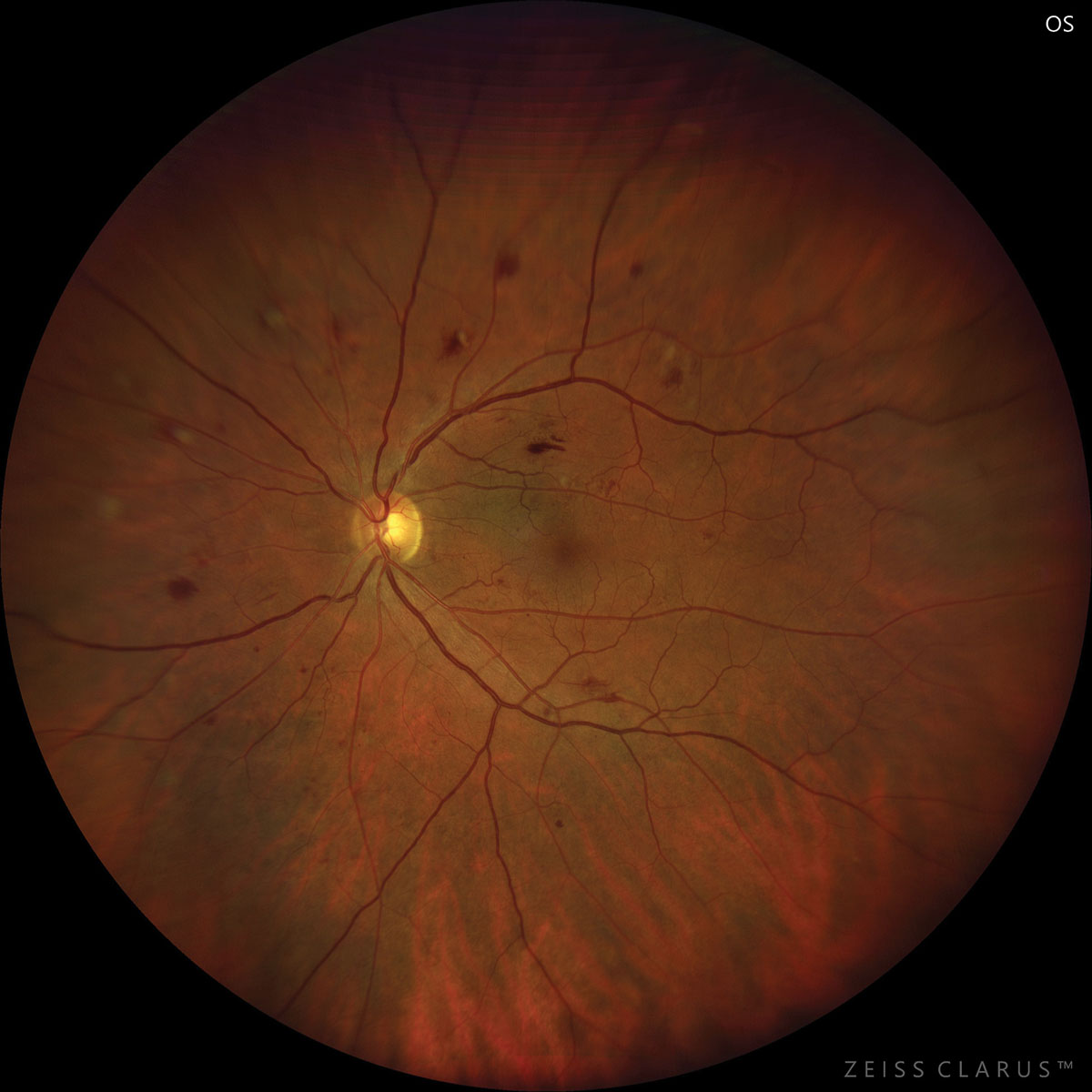
| Diabetic retinopathy developed in about 14% of diabetes patients followed for 6.5 years, regardless of whether or not aspirin use was a part of the patient’s daily regimen. Photo: Julie Torbit, OD. Click image to enlarge. |
Preclinical studies have indicated a potential role for chronic aspirin use in prevention of diabetic eye disease, but current findings from randomized trials are more sobering. In a new study appearing in Ophthalmology, researchers conducted a double-blind, randomized and placebo-controlled trial to test the results seen preclinically in prior investigations. This study was a sub-study of a trial called A Study of Cardiovascular Events iN Diabetes (ASCEND).
Included in the investigation were 15,480 UK adults aged 40 years or older with diabetes. Of those, linkage data was obtained for 7,360 (48% of those randomized in ASCEND). Over a mean follow-up of 6.5 years, 14.6% had a referable disease event in the aspirin group (100mg daily), defined as referable diabetic retinopathy (DR) or maculopathy based on grading criteria defined by the UK National Screening Committee. This percentage was extremely similar to that of the placebo group, demonstrating 14.2% that experienced a referable disease event.
Even further, there was no significant difference in proportion of sight-threatening eye bleed events, with the aspirin group experiencing this in 0.7% of cases, while placebo subjects in 0.8% of cases. The aspirin also had no effects on secondary or tertiary outcomes comparing referable disease stratified by baseline DR severity, progression in retinopathy grade, incident diabetic maculopathy or duplex retinopathy grades at final eye screening record.
The study authors point to their results building off evidence from the ETDRS study, in which 650mg of aspirin taken daily for seven years did not prevent development of high-risk proliferative features in 3,711 DR patients. There was a subgroup analysis (not adjusted for multiple comparisons) indicating that aspirin had no significant effects on incident maculopathy events in eyes assigned to either schedule in ETDRS. In the tertiary analyses for ASCEND, however, there was a trend toward harm on incident maculopathy, but the researchers explain this should be given cautious interpretation, since multiple comparisons were present.
The ASCEND eye study was a better test of aspirin at an earlier DR stage, since in the ETDRS study, participants already underwent pathological changes beyond cascading events at baseline. That is, the events of retinal capillary occlusion due to platelet thrombi or inflammatory changed involving the vascular endothelium are both identified triggers for a chain of events causing ocular diabetic microangiopathy. The dose of aspirin used in ASCEND was enough to inhibit certain agents, effectively lowering risk of vasoconstriction and platelet thrombosis. This may not have been enough to suppress an inflammatory mechanism of disease, though.
Although their results were null, the authors still convey the clinical relevance of their research: “For the first time, we have shown the feasibility of using the routinely collected retinopathy screening data to define outcomes in a large randomized trial. We have also introduced a new, clinically relevant way of defining the severity of eye-bleeding events, which other studies could adopt.”
At the very least, “these randomized data exclude any clinically meaningful effects of aspirin for DR but provide reassurance regarding the ophthalmological safety of aspirin.”
Sammons EL, Buck G, Bowman LJ, et al. ASCEND-Eye: effects of aspirin on diabetic retinopathy. Ophthalmology. January 16, 2024. [Epub ahead of print]. |

