 |
With the recent approval of Syfovre (pegcetacoplan injection, Apellis Pharmaceuticals) for dry age-related macular degeneration (AMD)/geographic atrophy (GA), we have a great opportunity to lead and individualize patient management. Each stage has various treatment options and knowing them may prevent permanent vision loss. Let’s review the stages and options, as well as the symptoms to look for and the most effective instruments to use.
Early AMD
This can be a difficult stage to identify, as few visual cues may be present. For many patients, the only symptoms might include difficulty with driving at night (contrast sensitivity loss) or difficulty recovering vision after entering a darkened room such as a theater (dark adaptation). Testing may consist of contrast sensitivity testing (M&S Technologies) or dark adaptation (AdaptDx Pro, Maculogix). Management focuses on lifestyle changes—smoking cessation, improving nutrition and taking formulations such as vitamins (e.g., Ocuvite, MacuHealth) or whole body nutrition supplements with antioxidants (e.g., OcularProtect, ProMacular Defense).
Intermediate AMD
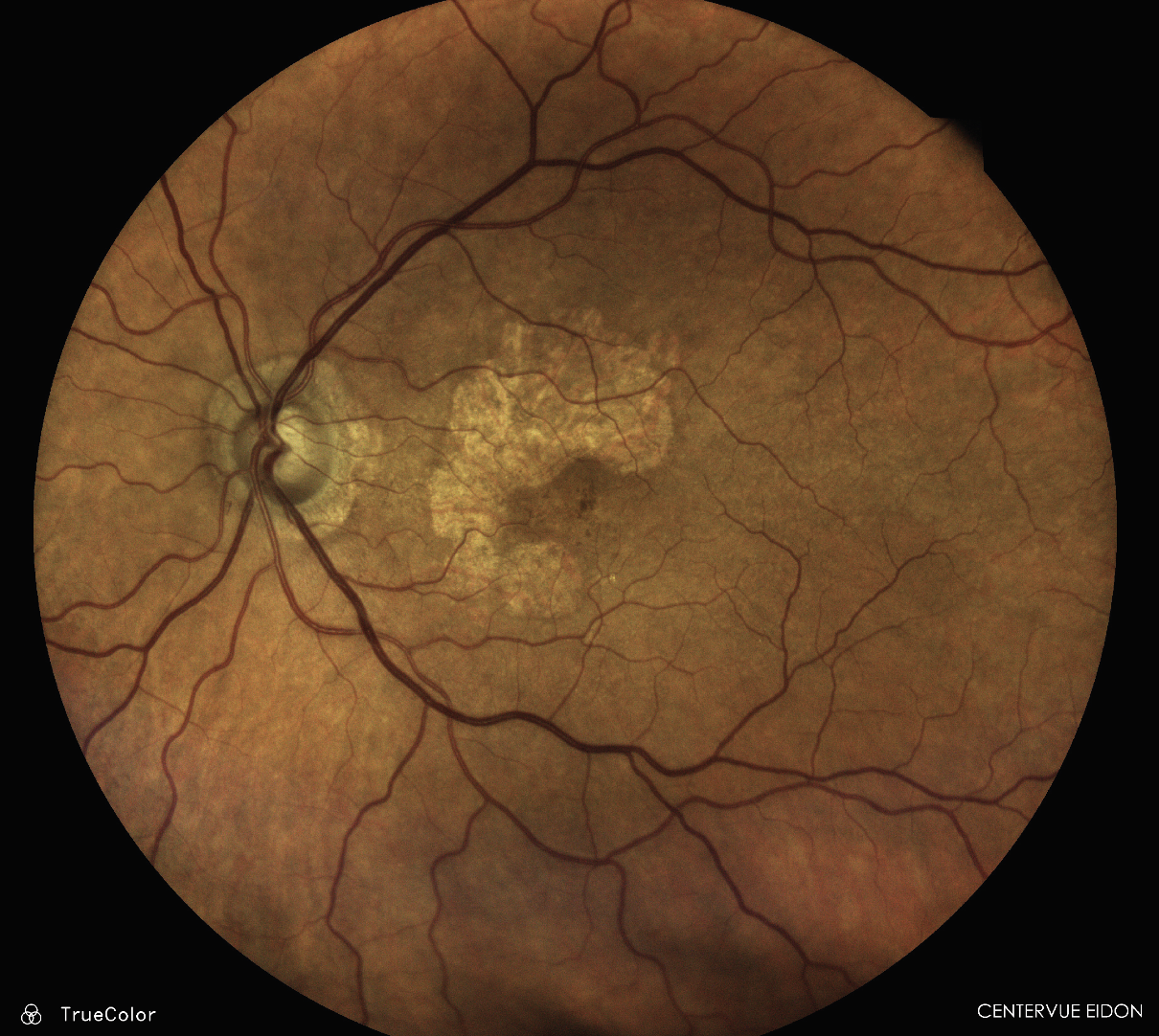
Symptoms sometimes increase at this stage, affecting reading and even visual acuity. Research has shown that AREDS II formulations (e.g., Preser-Vision) slow progression. Patients should be monitored regularly for wet AMD changes (e.g., ForeseeHome, Notal Vision) or GA development through more frequent OCT and high-resolution color fundus photography with blue-light fundus autofluorescence (FAF) imaging (e.g., iCare, Eidon). Higher risk of conversion to neovascular AMD may be indicated by drusenoid material that are large, soft or subretinal.
 |
|
GA, easily identified with the iCare Eidon Widefield TrueColor Confocal scanner. Click image to enlarge. |
Neovascular/Wet AMD
Fluid under the macular is best observed via OCT as either intraretinal or subretinal fluid, with pigment epithelial detachments. En face imaging may help visualize the neovascular net. OCT is critical at this stage and referral to a retina specialist for anti-VEGF injections is required.
GA
The approval of Syfovre and a pending approval later this year for Zimura (Iveric Bio) for a second complement system inhibitor gives hope to patients with dry AMD. These therapeutics were shown to slow progression of GA, but the hope is that after slowing progression of the devitalized cells/photoreceptors/retinal pigment epithelium (RPE), healthy cells in adjacent areas will avoid atrophy altogether. It is up to us to determine when to refer patients to a retina specialist for these injections.
While most GA occurs in patients with dry AMD, candidates also include patients with wet AMD who have been treated with anti-VEGF and experience significant drying. Starting with a 90D or 78D condensing lens or fundus photography helps determine if FAF or OCT should be ordered. FAF can help identify GA lesions through hyperfluorescence. Certain GA patterns, such as a patchy pattern (lesions greater than 200µm) or a diffuse pattern, are more prone to faster progression.
OCT is yet another effective way to determine ideal GA candidates, which show hypertransmission—like a barcode pattern—indicating atrophic areas of absent RPE. Patients with fovea-sparing lesions are excellent candidates, although they may not be identified due to maintaining good vision. Patients with central GA may still make good candidates if it’s not late-stage AMD.
Late-stage AMD
If the patient has passed the point of treatment options such as Syfovre, there’s still hope. From a surgical referral standpoint, there is the implantable miniature telescope (Samsara Vision), which is an IOL for cataract lens replacement that magnifies the image 2.7x, obtaining three to four lines of vision on average. A spectacle option includes AR technology that moves the object off the central macular scotoma (Eyedaptic). Finally, if none of these are possible, such as a patient who’s already had cataract surgery, refer them to a low vision specialist.
Dr. Karpecki is medical director for Keplr Vision and the Dry Eye Institutes of Kentucky and Indiana. He is the Chief Clinical Editor for Review of Optometry and chair of the New Technologies & Treatments conferences. A fixture in optometric clinical education, he consults for a wide array of ophthalmic clients, including ones discussed in this article. Dr. Karpecki's full list of disclosures can be found here.
