11th Annual Cornea ReportThe April 2024 issue of Review of Optometry highlights some hot topics in cornea, from keratoconus assessment and monitoring, to advancements in endothelial surgery, to causes and treatments of corneal pain. Check out the other articles featured in this issue:
|
Over the last few years, there have been radical changes in the treatments for corneal endothelial disease that have impacted the care optometrists provide to their patients. The most common cause of endothelial dysfunction is Fuchs’ dystrophy, which initially causes deposits on the posterior surface of the cornea called guttae (Latin for drops). Like rain drops on a windshield, they decrease vision, cause glare and even distort or diminish color vision. As Fuchs’ progresses, stromal edema develops—often worse in the morning—and like other forms of endothelial dysfunction, the edema causes even more visual loss, just like fog on a windshield.
As our treatments evolve and become more effective for Fuchs’ dystrophy and other forms of endothelial dysfunction, intervention often occurs much earlier in the disease process. For instance, we sometimes perform Descemet’s membrane endothelial keratoplasty (DMEK) for patients with 20/20 vision in a dark room assessed with our typical high contrast Snellen charts. In fact, studies have shown that visual outcomes tend to be better with earlier intervention.
This article will describe where we are with these treatments, what’s on the horizon and where they fit into care of these conditions.
The Gold Standard
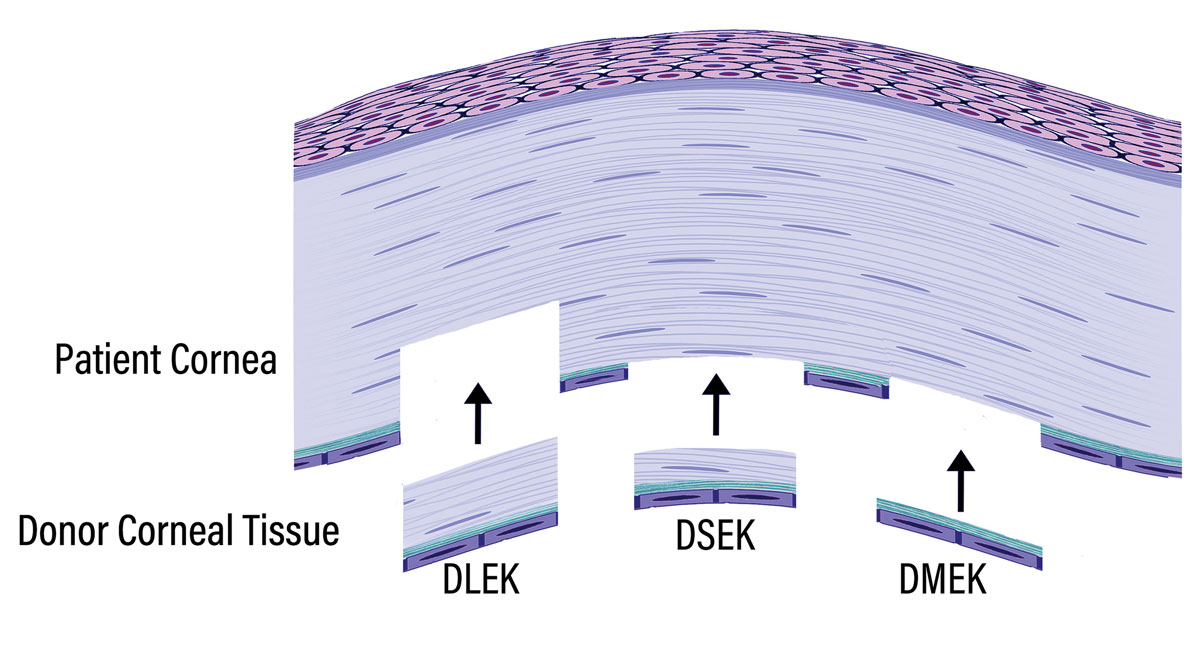
Endothelial keratoplasty (EK) has become the surgery of choice for corneal endothelial dysfunction. First introduced in 1998 by Gerrit Melles, MD, PhD, these techniques evolved from deep lamellar endothelial keratoplasty (DLEK) to Descemet’s stripping endothelial keratoplasty (DSEK) to DMEK, as the layers of host tissue that were removed and the layers of donor tissue that were implanted became increasingly selective (Figure 1).1,2 The current two EK techniques in widespread use—DMEK and DSEK—have led to faster visual recovery, better vision outcomes and substantially lower risk of complications.
The primary difference between DMEK and DSEK is that the former consists of healthy donor endothelium and Descemet’s membrane, whereas DSEK also includes some posterior stromal tissue (Figure 1). Key advantages of the DMEK procedure are that it provides faster visual recovery and has lower risk of immunologic rejection, whereas the thicker DSEK donor tissue tends to adhere more readily to the host cornea and is easier for the surgeon to manipulate. As reported in the Journal of Eye Banking and Corneal Transplantation, DMEK and DSEK comprised nine out of 10 grafts performed for endothelial disease in 2022, while penetrating keratoplasty (PK) accounted for only one out of 10.3 It is therefore important for eyecare professionals to understand these techniques and how to manage pre- and postoperative care.
The most important preoperative consideration is that early intervention with EK is associated with better visual outcomes, because, over time, corneal edema leads to stromal and epithelial fibrosis. The epithelium can be removed during EK to treat map-dot-fingerprint or anterior basement membrane dystrophy, but the stromal tissue is not replaced, so any stromal fibrosis will adversely affect postoperative vision.4 Overall, EK is a small-incision procedure with an excellent safety profile; the benefits of early intervention typically outweigh the risks.
 |
|
Fig. 1. Schematic illustrating the relative thickness and layers of recipient tissue removed and donor tissue implanted in successive iterations of EK known as DLEK, DSEK and DMEK. Note that DLEK includes removal of recipient posterior stroma, Descemet’s membrane and endothelium whereas only the central host Descemet’s membrane and endothelium are removed in DSEK and DMEK. Click image to enlarge. |
Fuchs' Dystrophy: Clinical Considerations
As mentioned previously, Fuchs’ endothelial corneal dystrophy (FECD) is the leading indication for EK in the United States, followed by corneal edema after cataract surgery.3
One of the first symptoms patients notice is glare from the guttae (Figure 2). Even those who can see relatively well on a standard eye chart in a darkened room often experience glare that interferes with activities of daily living, such as driving at night, working under fluorescent lights or being outdoors on a bright, sunny day. Corneal edema and lens changes can also contribute to glare, but we can’t overlook the contribution of the guttae. In addition to a careful assessment of symptoms, a brightness acuity test is a useful tool in determining the level of glare in early FECD. Ask about their level of confidence in driving at night. Have they encountered difficulties or stopped driving at night all together? Is their spouse afraid to ride in a car with them if they are driving?
As FECD progresses, corneal endothelial cells loss continues. Eventually, the remaining cells become unable to maintain optimal corneal hydration, resulting in stromal edema, which disrupts the stromal collagen spacing. This increases light scattering and leads to clinical complaints of blurry vision, especially in the morning. Pachymetry should be used to monitor corneal thickness changes. As edema becomes more significant, thickness will increase and the patient can have painful bullae and scarring occur. With the rapid vision recovery that comes with EK procedures, reduction in glare and improvement in color vision, eyecare providers should consider referring patients early for surgical intervention.
Patients with visually significant Fuchs’ dystrophy often have cataracts as well. Most prefer to have the cataract surgery and Fuchs’ treatment at the same time instead of undergoing separate surgical procedures. EK can be performed simultaneously with cataract surgery, using the same main incision for the DMEK procedure or enlarging it slightly for DSEK. However, corneal guttae and edema affect the imaging used to determine the optimal intraocular lens power, so refractive outcomes are less predictable when cataract surgery is combined with EK than they are when cataract surgery is performed alone in eyes with normal corneas. While there is an average shift towards hyperopia (about 0.5D) after EK because of posterior corneal curvature steepening associated with resolution of edema, either a myopic or hyperopic shift can occur from what was predicted (range -2.00D to +3.00D). Methods to optimize refractive outcomes are later discussed in the Visual Outcomes section.
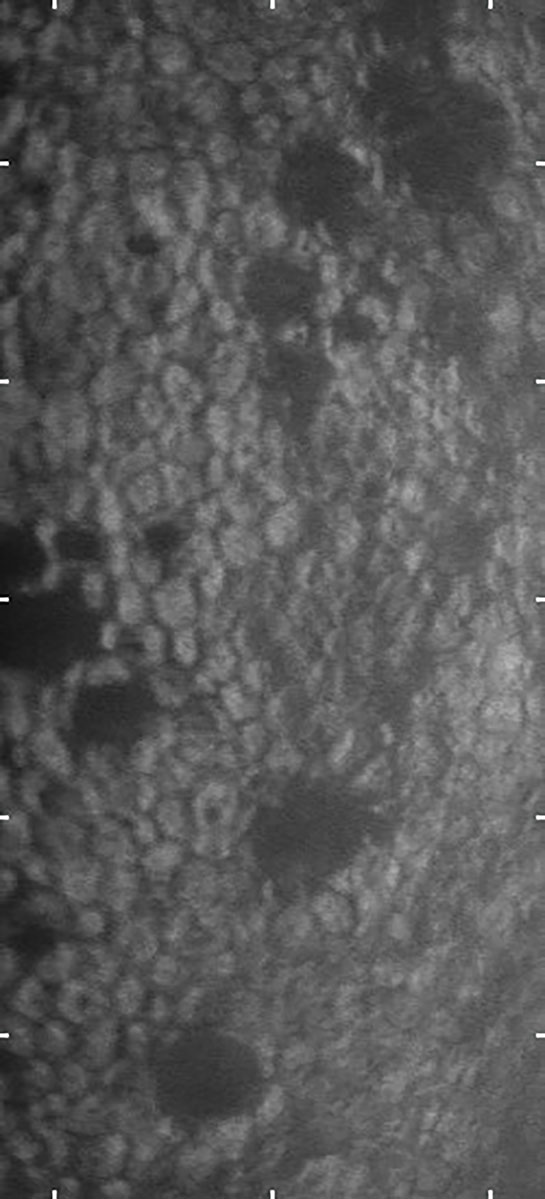 |
Fig. 2. Specular microscopy image of the corneal endothelium in a patient with early Fuchs’ dystrophy. The dark areas are the characteristic guttae associated with endothelial cell drop out. Click image to enlarge. |
Additional Indications
The other leading indications for EK are bullous keratopathy and failed previous keratoplasty.3 Each year approximately four million cataract procedures are performed in the US, and about 4,000 keratoplasty procedures are performed to treat corneal edema following cataract surgery. An increasing cause of endothelial failure is secondary corneal edema after glaucoma filtration surgery, especially tube shunts. Among the approximately 50,000 keratoplasty procedures performed each year in the US, over 10% are regrafts, primarily to treat endothelial decompensation.3
Less common conditions that can be treated with EK include post-infectious endothelial dysfunction, iridocorneal endothelial syndrome, polymorphous corneal dystrophy and congenital hereditary endothelial dystrophy. EK can be performed in eyes with challenging anterior chamber anatomy (e.g., glaucoma tube shunts, aniridia and aphakia) with appropriate modifications. Surgeons often prefer DSEK over DMEK in unicameral eyes because the thicker DSEK tissue can be suture fixated to the host cornea to prevent migration into the posterior chamber.
 |
|
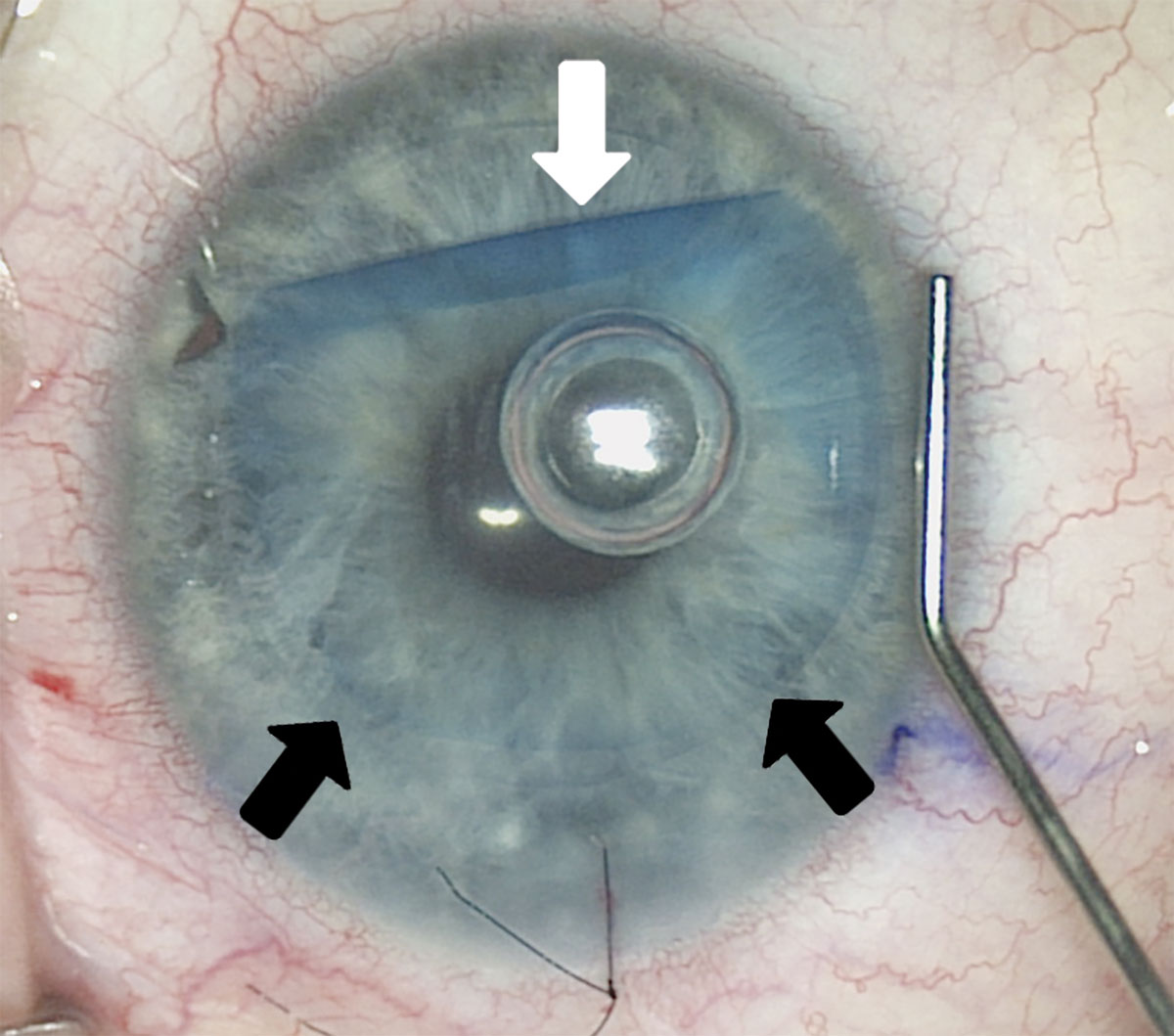
Fig. 3. This intraoperative image shows placement of DMEK donor tissue in a recipient eye. The DMEK tissue, which is approximately 20µm thick, was stained with trypan to facilitate visualization. The tissue was folded for insertion through a 2.2mm incision, and is being uncurled inside the eye using tapping maneuvers on the surface of the host cornea. A small air bubble was injected beneath the DMEK tissue to help it stay uncurled and pressed against the host cornea. The black arrows show the thin edge of the graft where it is fully uncurled and the white arrow shows an edge that is still curled. Click image to enlarge. |
Post-Surgical Care
Clinically, there are four things to watch for after EK surgery: pupillary block, graft detachment, steroid-induced intraocular pressure (IOP) rise and immunologic graft rejection. Surgeons often create an inferior peripheral iridotomy to prevent pupillary block and leave a large air bubble in the eye at the end of the case. Before sending the patient home after surgery, examine the eye at the slit lamp to ensure the peripheral iridotomy is patent and the IOP is within the normal range.
Edge detachment is the most common early postoperative complication (Figure 4). A DSEK graft includes posterior donor stromal tissue, which tends to adhere more readily to the host cornea than a DMEK graft. Corneal surgeons typically follow EK patients closely in the first week to assess attachment, and they may ask patients to lay on their back as much as possible for the first day or so—particularly after DMEK—to allow the bubble to press the graft against the host cornea.
If over one-third of the graft is detached, an area of detachment seems to be increasing or detachment extends into the visual area, the surgeon can reinject air or gas into the eye to promote attachment. Re-bubble rates commonly vary from 5% to 25%, depending upon specific techniques used, as well as donor and host factors.5 Patients may return to the optometrist’s care with small edge detachments that just need to be monitored. These will resolve over time, but if the area of detachment appears to be increasing or affecting vision, referral back to the surgeon is warranted.
Topical corticosteroids are used after EK to prevent graft rejection, with the dosage and tapering schedule varying among corneal surgeons. The most common side effect of prolonged topical steroid use is IOP rise (patients with pre-existing glaucoma are particularly susceptible). Monitor pressures closely, especially in the first three to six months post-surgery due to higher initial steroid dosing, which is tapered over time. Prospective, randomized studies have shown that the topical steroid strength can be safely reduced one month after EK or two months after EK combined with cataract surgery, from prednisolone acetate 1% to fluorometholone 0.01% or loteprednol 0.5%.6,7 This early steroid reduction substantially reduces the risk of IOP elevation. Patients that remain on steroids of any dose should be followed at least every six months to monitor IOP.
An advantage to EK is that episodes of rejection are significantly less than with PK. One study reported rejection rates of 1.7% with DMEK, 5% with DSEK and 14% with PK in a five-year study in grafts that were performed for FECD and bullous keratopathy.8 Preventing immunologic graft rejection is the reason behind keeping keratoplasty patients on topical steroids long-term. Rejections in EK patients, especially DMEK, can be subtler than in PK eyes. Increase in pachymetry in the absence of any other signs is an indicator of rejection and should be treated with increased topical steroids. Less common signs of rejection in EK include redness, pain, increased stromal haze and keratic precipitates. Knowing your surgeon’s protocol for steroid use is important for the long-term care of EK patients.
Visual Outcomes
EK provides rapid visual rehabilitation and excellent long-term visual outcomes. With DMEK, about 70% of patients achieve 20/25 or better best-corrected visual acuity (BCVA) within three months and over half have 20/20 or better BCVA at five years and 10 years in the absence of other vision-limiting ocular co-morbidity. The median BCVA tends to be about one line less with DSEK because DSEK tissue is slightly thicker and more likely to increase higher order aberrations on the posterior corneal surface.5 EK has also been shown to improve color vision and discernment.9
Given these impressive BCVA outcomes, FECD patients are increasingly interested in optimizing uncorrected visual acuity (UCVA) with EK and concurrent or staged cataract surgery. The challenge is that the corneal changes associated with FECD distort the biometry measurements used to determine the optimal intraocular lens power, so it is harder to hit the refractive target and optimize UCVA in FECD patients.
Two approaches can be taken to optimize UCVA in FECD patients. The first is to combine DMEK with cataract surgery and implant an intraocular lens that can be adjusted postoperatively. In our study of this approach, we found that 90% of the treated eyes achieved UCVA of 20/25 or better and 100% had UCVA of 20/40 or better.10 Another way to optimize UCVA is to perform DMEK, allow the cornea to stabilize, do the biometry measurements and then perform cataract surgery. This approach allows implantation of a presbyopia-correcting intraocular lens in patients who want to minimize the need for glasses.
EK Surgery at a GlanceThe key elements of EK surgery are:
The air bubble naturally dissipates over several days. Some surgeons prefer to use a gas mixture that remains in the eye longer. |
Two types of presbyopia-correcting lenses are approved in the US: extended depth of focus and multifocal. The latter design provides better near vision but is associated with more visual phenomena, such as glare and halos, so some surgeons avoid multifocal lenses in Fuchs’ dystrophy eyes. We found that DMEK followed later by cataract surgery and implantation of a presbyopia-correcting lens resulted in median BCVA of 20/20 (range 20/15 to 20/25), median binocular UCVA of 20/25 (range 20/15 to 20/25) and median binocular uncorrected near vision of 20/20 (range 20/20 to 20/50).11
Graft Survival
Long-term EK survival equals or exceeds that PK when performed by experienced surgeons, although the EK learning curve is associated with increased risk of early graft failure. In large, prospective, multi-center US clinical studies with experienced surgeons, the graft success rate at three years was 94% with DSEK and 92% with PK for treatment of similar indications.12 Five-year survival rates of DMEK and DSEK performed for FECD at two large referral centers ranged from 93% to 97%.8,13
The principal patient characteristics that influence EK survival are the indication for grafting and prior glaucoma filtration surgery. Patients with relatively functional peripheral corneal endothelium, such as FECD patients, generally have better long-term graft survival than those with dysfunctional peripheral endothelium, such as patients with pseudophakic or aphakic corneal edema. Pre-existing medically managed glaucoma moderately increases the risk of graft failure. Prior glaucoma filtration surgery, including trabeculectomy or aqueous tube shunt, substantially increases the risk of failure such that those patients should be advised that their graft may need to be replaced within five years.14 Fortunately, it is straightforward to remove a failed EK and replace it through a small incision.
New Treatments on the Horizon
Currently, EK is the gold standard for treating corneal endothelial dysfunction, as it safely provides rapid visual rehabilitation and has excellent long-term outcomes. The US harvests an adequate supply of donor tissue to meet domestic needs, but most other countries in the world do not. Therefore, alternative approaches that could help address the worldwide shortage of donor tissue are being evaluated in US clinical trials. These include a surgical technique called Descemet’s stripping only (DSO), injection of cultured human corneal endothelial cells and pharmacologic or biologic eye drop treatments.
In patients with FECD, the deposition of guttae and endothelial cell dropout often begin centrally, and some patients with symptomatic FECD still have healthy peripheral corneal endothelium. DSO removes central Descemet’s membrane and endothelium without implanting any donor tissue. It can be used in selected patients with early-stage FECD who still have healthy peripheral endothelium that can migrate over and cover the denuded area. The clearing rate varies substantially between patients, and we do not yet have a way to predict who will be a rapid responder, a slow responder or a non-responder.
Studies have shown that the likelihood of successful clearing improves if the area of stripping is limited to 4.5mm or less (this is only 25% as much area as is removed with EK).15 Early-stage clinical trials have shown that two approaches—either injection of a growth factor at the time of DSO or use of a rho-kinase inhibitor eye drop for several months post-op—can help with corneal clearing.16 Studies suggest that ripasudil, a rho-kinase inhibitor approved in Japan for treatment of glaucoma, may be more effective after DSO than netarsudil, the rho-kinase inhibitor approved in the US for that purpose. Ripasudil is currently being evaluated in US clinical trials for use with DSO (NCT05795699 and NCT05826353 on ClinicalTrials.gov).
Compared with EK, the main advantages of DSO are that it does not require donor tissue or long-term use of topical corticosteroids to prevent rejection. Main disadvantages are that it’s limited to early-stage FECD patients and visual rehabilitation tends to be slower and less predictable. Approximately one in 10 eyes do not fully clear after DSO and require rescue with EK.
Human corneal endothelial cells can be expanded in the laboratory, allowing cells derived from a single donor cornea to be used to treat 100 or potentially up to 1,000 patients.17 Several companies are conducting clinical trials in the US to evaluate cell injection therapy.
Clinical trials are also underway to evaluate eye drop treatments that could potentially slow or halt the progression of FECD. Treatments that target the most common genetic marker in FECD, a trinucleotide repeat expansion in the TCF4 gene, are also in development. While DSO costs substantially less than EK because it does not require any donor tissue, we don’t know yet how the cost of cell injection therapy, pharmacologic or genetic treatments will compare with EK, which for most patients is a one-time treatment that provides excellent visual rehabilitation.
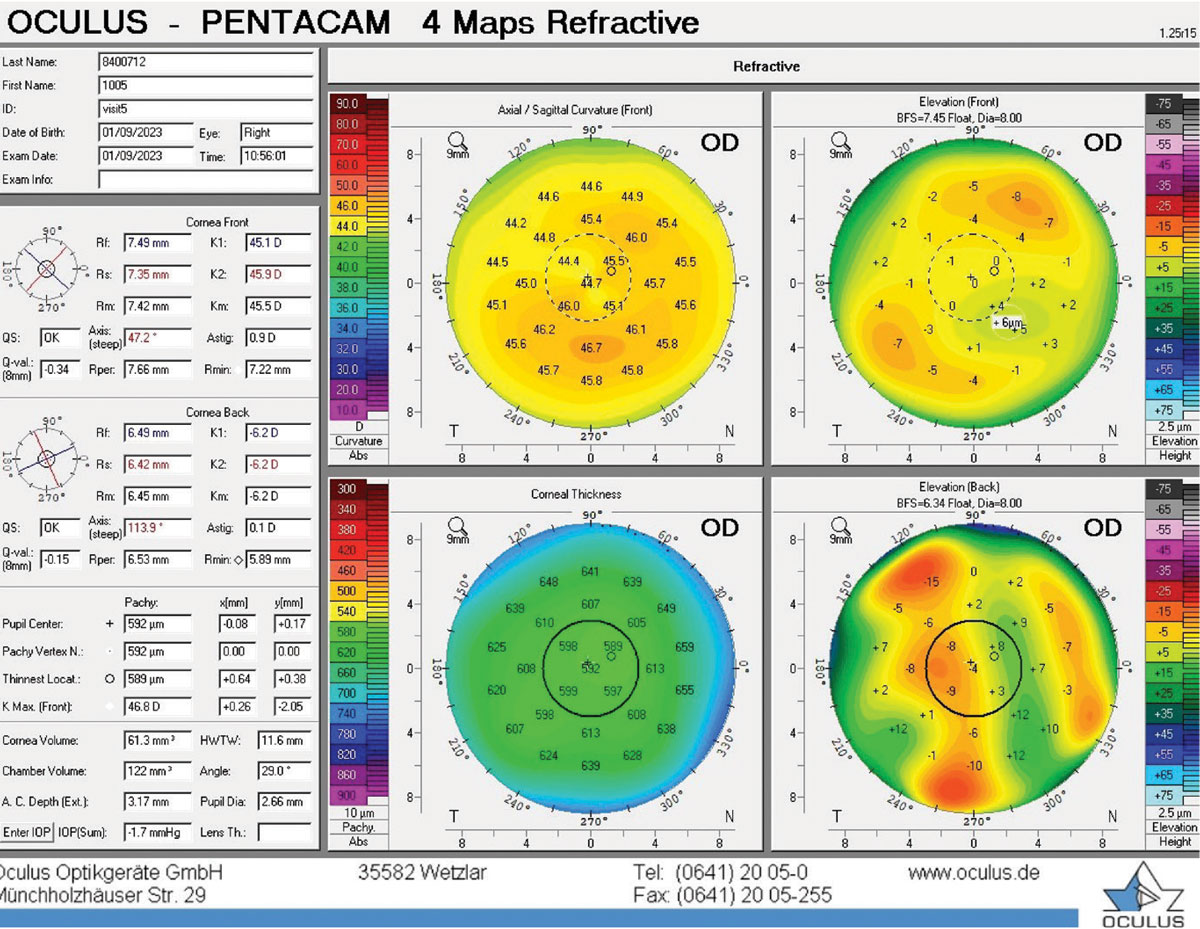 |
Pentacam image of posterior corneal irregularities and displacement of thinnest point in Fuchs’ dystrophy. Click image to enlarge. |
Takeaways
Proper diagnosis and management of all corneal conditions are key to ensure favorable outcomes for patients. When conservative measures and noninvasive treatments are insufficient, prompt referral to ophthalmology and effective comanagement is vital for success.
Dr. Kelley practices at Price Vision Group in Indianapolis, IN, and is experienced in caring for complicated corneal transplant patients and laser refractive surgery patients. She has served as a sub-investigator in numerous clinical trials and coordinated the clinical studies on artificial irises and the intraocular lenses for high levels of nearsightedness. Dr. Francis Price, Jr., is founder and president of Price Vision Group and the Cornea Research Foundation of America. He is also the president and co-founder of the Medical Practice Consortium, a nonprofit organization providing health insurance benefits to 90 independent group medical practices who are members of the Indiana State Medical Association. He has authored over 250 peer-reviewed publications and book chapters and been principal investigator of more than 130 clinical studies of ophthalmic devices, medications and surgical techniques. Dr. Marianne Price is executive director of the Cornea Research Foundation of America in Indianapolis, IN. She holds a PhD in Medical and Molecular Genetics from Indiana University School of Medicine. Dr. Price has authored over 150 peer-reviewed publications and book chapters and made presentations to vision care audiences around the world.They have no financial disclosures.
1. Melles GR, Eggink FA, Lander F, et al. A surgical technique for posterior lamellar keratoplasty. Cornea. 1998;17:618-26. 2. Price MO, Mehta JS, Jurkunas UV, Price FW Jr. Corneal endothelial dysfunction: evolving understanding and treatment options. Prog Retin Eye Res. 2021;82:100904. 3. Mathews P, Benbow A, Corcoran K, et al. 2022 eye banking statistical report—executive summary. Eye Bank Corneal Trans. 2023;2(3):e0008-12. 4. Letko E, Price DA, Lindoso EM, et al. Secondary graft failure and repeat endothelial keratoplasty after Descemet’s stripping automated endothelial keratoplasty. Ophthalmology. 2011;118(2):310-4. 5. Chamberlain W, Lin CC, Austin A, et al. Descemet endothelial thickness comparison trial: a randomized trial comparing ultrathin Descemet stripping automated endothelial keratoplasty with Descemet membrane endothelial keratoplasty. Ophthalmology. 2019;126(1):19-26. 6. Price MO, Price FW Jr, Kruse FE, et al. Randomized comparison of topical prednisolone acetate 1% vs fluorometholone 0.1% in the first year after Descemet membrane endothelial keratoplasty. Cornea. 2014;33(9):880-6. 7. Price MO, Feng MT, Scanameo A, Price FW Jr. Loteprednol etabonate 0.5% gel vs. prednisolone acetate 1% solution after Descemet membrane endothelial keratoplasty: prospective randomized trial. Cornea. 2015;34(8):853-8. 8. Woo JH, Ang M, Htoon HM, et al. Descemet membrane endothelial keratoplasty vs Descemet stripping automated endothelial keratoplasty and penetrating keratoplasty. Am J Ophthalmol. 2019;207:288-303. 9. Price DA, Price MO, Lopez A, Price FW Jr. Effect of Descemet membrane endothelial keratoplasty on color vision in patients with Fuchs dystrophy. Cornea. 2016;35(8):1045-8. 10. Price DA, Dudasko KN, Hall TA, et al. Initial results of DMEK combined with cataract surgery and implantation of the light adjustable lens. J Cataract Refract Surg. 2024;50(3):270-5. 11. Price MO, Pinkus D, Price FW Jr. Implantation of presbyopia-correcting intraocular lenses staged after Descemet membrane endothelial keratoplasty in patients with Fuchs’ dystrophy. Cornea. 2020;39(6):732-5. 12. Rosenwasser GO, Szczotka-Flynn LB, Ayala AR, et al. Effect of cornea preservation time on success of Descemet stripping automated endothelial keratoplasty: a randomized clinical trial. JAMA Ophthalmol. 2017;135(12):1401-9. 13. Price DA, Kelley M, Price FW Jr, et al. Five-year graft survival of Descemet membrane endothelial keratoplasty (EK) vs Descemet stripping EK and the effect of donor sex matching. Ophthalmology. 2018;125:1508-14. 14. Anshu A, Price MO, Price FW. Descemet’s stripping endothelial keratoplasty: long-term graft survival and risk factors for failure in eyes with preexisting glaucoma. Ophthalmology. 2012;119:1982-7. 15. Borkar DS, Veldman P, Colby KA. Treatment of Fuchs’ endothelial dystrophy by Descemet stripping without endothelial keratoplasty. Cornea. 2016;35(10):1267-73. 16. Moloney G, Petsoglou C, Ball M, et al. Descemetorhexis without grafting for Fuchs’ endothelial dystrophy-supplementation with topical ripasudil. Cornea. 2017;36(6):642-8. 17. Kinoshita S, Koizumi N, Ueno M, et al. Injection of cultured cells with a ROCK inhibitor for bullous keratopathy. N Engl J Med. 2018;378(11):995-1003. |

