 |
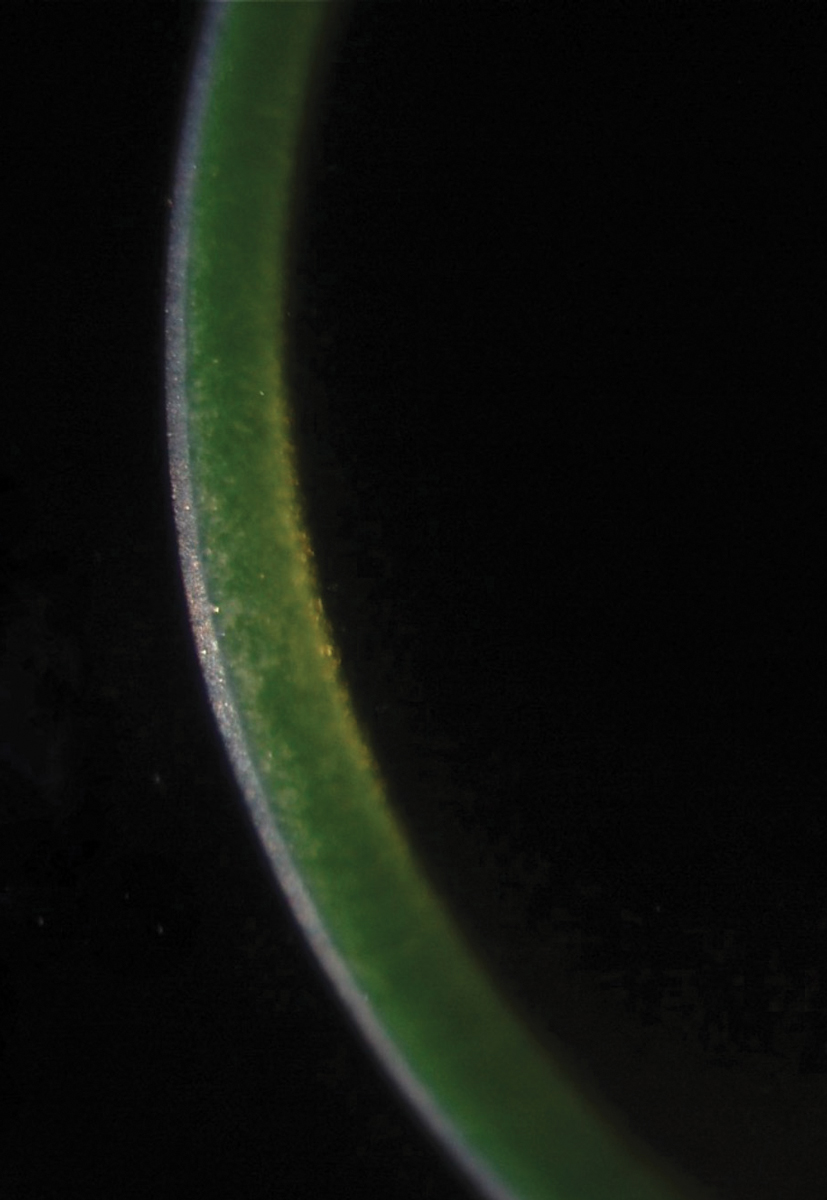
| The green glow of riboflavin indicates adequate penetration into the corneal stroma prior to collagen crosslinking. Photo: Roy Rubinfield, MD. Click image to enlarge. |
Corneal crosslinking (CXL) has quickly become an integral part of early keratoconus management, but many doctors and patients find the procedure—with multiple applications of riboflavin and UVA light over a 30-minute period—tedious and inefficient. Investigators have been studying a faster protocol known as accelerated crosslinking (ACXL). A recent study describes its efficacy in stabilizing keratoconus over prolonged observation times. A German team found a significant improvement of functional and tomographical results post-ACXL over a follow-up period of 56 months.
A total of 74 eyes of 53 patients with progressive keratoconus who underwent ACXL (18mW/cm2 for five minutes) were included, with the investigation focused on tomographic and keratometric parameters, refractive data and visual outcomes at nearly five years post-procedure.
Corrected distance visual acuity, slit lamp and Pentacam examinations were conducted two weeks before the surgery and, on average, 56 months after the surgery, and included assessments of thinnest corneal point, minimum radius, corneal astigmatism and maximum anterior keratometry (Kmax). In a subgroup of 24 eyes, Pentacam examination data from an intermediate visit at 12 months until the final visit was evaluated to confirm continuous stability.
The ACXL protocol included corneal abrasion, riboflavin eye drops administered every five minutes for a total duration of 30 minutes and irradiation with 18mW/cm2 for five minutes using riboflavin eye drops applied every minute during the irradiation process. Intraoperatively, minimal corneal pachymetry of >400μm was ensured in every patient.
The team assessed the results to demonstrate statistically significant improvement. “Moreover,” they wrote in their paper on the study, “we observed stable conditions in patients with previously progressive keratoconus, including during the final year of the observation period. The treatment failure rate, defined as an increase in Kmax greater than 1D during the five-year follow-up, was 4%.”
ACXL has been associated with a shallower demarcation line compared to the conventional crosslinking protocol. However, accelerated crosslinking’s use of hydroxypropylmethylcellulose solution as a vehicle for riboflavin allows for faster intrastromal diffusion of the agent, resulting in a deeper demarcation line, the authors noted. “This deeper demarcation line has been shown to lead to greater topographic flattening compared to ACXL with dextran solution” used in conventional CXL, the authors explained.
Studies have also reported greater topographic flattening after ACXL in patients with initially steeper corneas (Kmax 54D or more). “Additionally, ACXL appears to be more effective in preventing progression in patients with advanced keratoconus,” the authors noted. “However, concerns have been raised about the reduced total amount of generated crosslinks in ACXL, leading to suspicion of reduced long-term stability.”
Friedrich J, Sandner A, Nasseri A, et al. Accelerated corneal cross-linking (18mW/cm2 for 5 min) with HPMC-riboflavin in progressive keratoconus – five years follow-up. Graefes Arch Clin Exp Ophthalm. August 26, 2023. [Epub ahead of print.] |

