 |
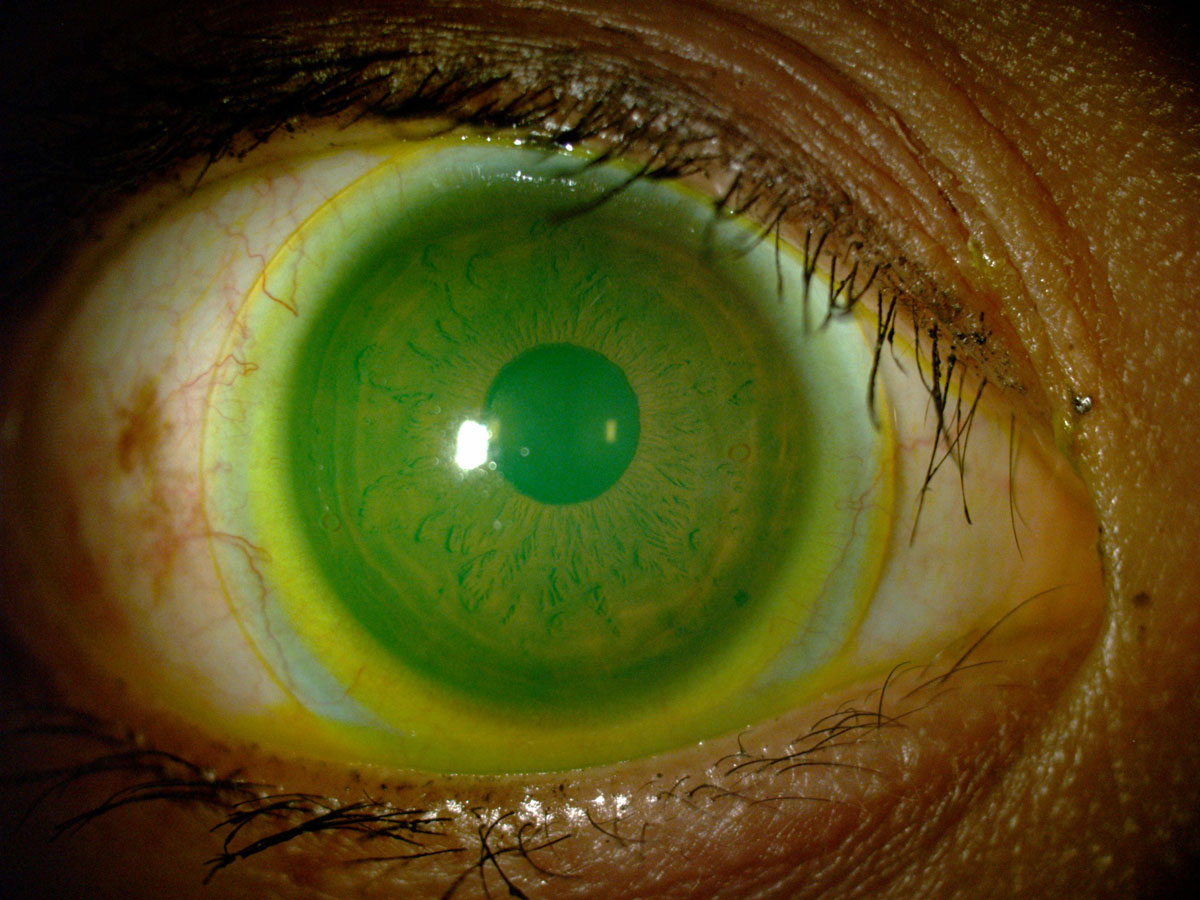
Scleral lens wear wasn't found to affect meibomian gland visibility in most cases. Click image to enlarge. |
Some literature suggests wearing soft and rigid contact lenses, including scleral lenses, may increase the risk of meibomian gland dropout and alter gland morphology and meibomian expressibility and quality, leading to dry eye. A recent study observed meibomian gland changes in scleral lens wearers over 12 months, and while the team did not find that these patients were adversely affected by meibomian gland dropout or visibility, they concluded that their method of assessment is objective and repeatable for use in further research.
A total of 43 patients were included in the study, all of whom had worn scleral lenses for one year. Each subject underwent infrared meibography of the upper eyelid, and results were divided into three groups:
Group 1: patients with good subjective gland visibility and an Image J dropout percentage less than one-third of the total area of meibomian glands
Group 2: patients with low subjective gland visibility and an Image J dropout percentage less than one-third of the total area
Group 3: patients with low subjective gland visibility and an Image J dropout percentage greater than one-third of the total area
The visibility metrics were calculated using a previously developed algorithm which was recently validated for the Keratograph 5M. “This algorithm is similar to the meibomian gland contrast measurement,” the researchers explained in their paper. “It was proven that, as meibomian glands are lighter than the background in a meibography, the visibility of meibomian glands could be used as a feature to aid in the assessment of those secretory structures. Moreover, another study found that meibomian gland visibility metrics have good sensitivity and specificity to diagnose MGD, with higher diagnostic capability than current diagnostic metrics such as meibomian gland dropout.” In addition, patients completed an Ocular Surface Disease Index (OSDI) questionnaire at baseline and after one year of scleral lens wear.
The researchers found that gland dropout percentage was not statistically different between groups 1 and 2, though group 1 showed the highest grey pixel intensity values of all three groups. They also concluded that gland visibility metrics and gland dropout percentages were significantly correlated, validating the efficacy of this proposed method for evaluating the alteration of meibomian glands in these patients.
“No statistically significant differences were found in meibomian gland dropout percentage and gland visibility metrics between baseline and after one year of scleral lens wear,” the researchers wrote. “Nevertheless, an average improvement in OSDI of 24.5 was found after one year of scleral lens wear. Thus, this might suggest that scleral lens wear appears to not adversely affect the meibomian gland dropout and visibility while promoting comfortable wear.”
Considering the relatively small sample size of the study and disagreement among existing studies, the researchers suggest that the link between gland dropout and gland function continue to be investigated and that the algorithm used in this study may be an effective tool in meibomian gland assessment.
“In the present study, an objective, semi-automatic algorithm based on the analysis of the visibility of meibomian glands, which was previously developed for the Keratograph 5M, was validated for a commercial fundus camera. Despite the algorithm being semi-automatic—since the region of interest of glands needs to be manually delimited—repeatability of gland visibility metrics showed to be moderate-acceptable,” the researchers concluded.
García-Marqués JV, Macedo-De-Araújo RJ, Cerviño A, et al. Assessment of meibomian gland drop-out and visibility through a new quantitative method in scleral lens wearers: a one-year follow-up study. Cont Lens Anterior Eye. January 5, 2022. [Epub ahead of print]. |


