 |
|
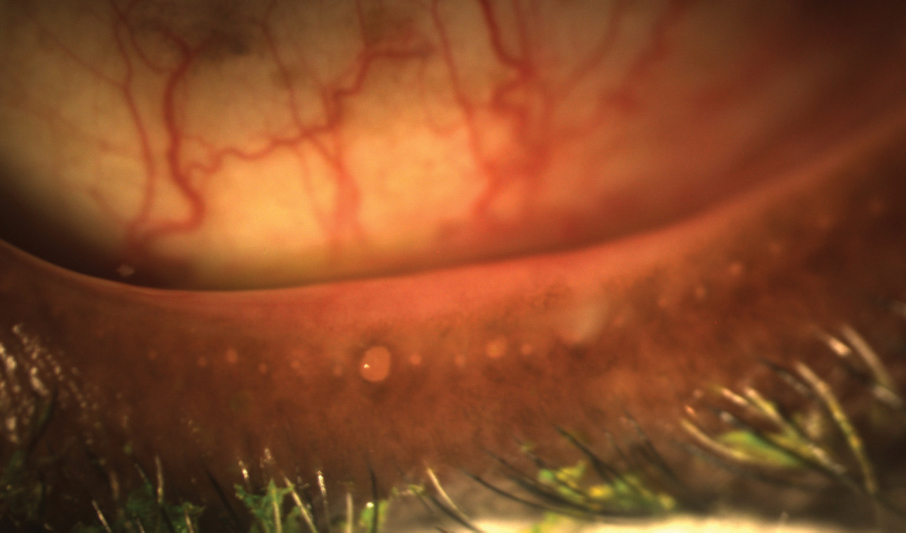
This study (and several before it) could not draw a definitive link between MGD and pregnancy, but hormones are one possible cause of MGD symptoms in some expectant mothers. Photo: Doan Huynh Kwak, OD. Click image to enlarge. |
Meibomian gland disease (MGD) is considered the leading cause of dry eye. It’s often missed, however, because most MGD is nonobvious obstructive MGD, and its clinical signs aren’t apparent except on lid expression. Dry eye assessment is shifting away from sequelae-based diagnoses and toward etiology-based diagnoses. As a result, experts say it’s “imperative” to study MGD among various populations such as pregnant women, for example. “Dry eye reported in pregnancy is attributed to the disruption of lacrimal gland acinar cells,” researchers noted in a recent study. “Little attention has been paid to MGD in pregnancy.”
The team pointed to a previous study that reported a high prevalence of dry eye among pregnant women, with the highest rate and the most signs and symptoms occurring in the third trimester. The lowest prevalence was found six weeks postpartum. “It’s not clear whether the occurrence of MGD in pregnant women is also high,” the researchers noted. “Because MGD has a leading causative role in dry eye, it will be worthwhile exploring its occurrence in pregnant women and determining factors that influence its occurrence.”
“Pregnancy generally creates significant metabolic changes throughout the body,” they explained further. “It increases the demand for metabolic fuels for fetal growth and perpetuates substantial hormonal changes in the body, which leads to changes in the lipid profile during different trimesters of pregnancy. Lipid levels have been shown to affect meibomian gland function.”
To examine MGD occurrence in pregnant patients and determine influential factors, the researchers conducted a hospital-based, cross-sectional study of 201 pregnant women. Each participant underwent meibomian gland assessment and tear function tests, as well as a symptom questionnaire. The investigators found that while pregnant people exhibited a high frequency of MGD, the prevalence was comparable to that reported in the normal population.
The frequency of MGD among the study cohort was 23%. The following factors were significantly associated with MGD: high-density lipoprotein (HDL), total cholesterol (TC) and low-density lipoprotein (LDL). However, MGD wasn’t significantly associated with any of the three.
“To the very best of our knowledge, no studies on MGD have been conducted on pregnant women in Ghana and elsewhere in the world,” the researchers said. They noted that the prevalence found in their study was within the range of the global reported frequency of MGD among clinical populations (20% to 61%).
Based on their findings of MGD occurrence, the researchers believe other factors are at work in women with dry eye. “The prevalence of dry eye is reported to skyrocket during the third trimester of pregnancy,” they said. “If dry eye in pregnant women has MGD as its sole causative factor, one would expect the occurrence of MGD to be high in the third trimester, which wasn’t the case. It may imply that the reported increase in dry eye occurrence with increasing gestational age (advancing trimester) could have other causative instigators aside from MGD.”
One possible reason for MGD in pregnant women is a suboptimal balance between testosterone and estrogen. “The physiological capabilities of the meibomian glands are maintained through an optimal and homeostatic balance between testosterone and estrogen,” they said. “Testosterone facilitates the maturation and differentiation of the meibomian glands, whereas estrogen promotes acinar cell death leading to a depletion in glandular secretions and the miniaturization of the glands. Pregnancy causes an elevation in estrogen, testosterone and progesterone levels, which is gradual but progressive with gestational age.”
The researchers explored several risk factors including fasting blood glucose, lipid profile, gravidity, BMI, gestational age and participant age. Though age is a known risk factor for MGD, it wasn’t significantly associated with MGD in this cohort, mainly due to the narrow age range (17 to 40), the researchers explained. “No other factor was associated with MGD except the lipid profile (TC, HDL and LDL), which showed a marginal risk of MGD in univariate analysis but lost significance in multivariate analysis. This is consistent with several studies that have demonstrated an association between hypercholesterolemia and MGD. Despite no factor being associated with MGD in multivariate analysis, one may undoubtedly argue that this may be because of collinearity between the lipid predictors of MGD, which may bias the multivariate binary logistic regression model.”
Overall, there was a high frequency of MGD in pregnant women, but this was comparable to a normal population. The researchers noted a marginal risk of MGD with an increasing level of cholesterol in pregnant women. “Clinicians examining women for dry eye disease may need to pay attention to other etiological instigators aside from MGD to enable the clinicians to make the appropriate etiology-based diagnosis,” they wrote.
| Kyei S, Asiedu K, Ephraim RKD, et al. Meibomian gland dysfunction and lipid profile: a study among pregnant women. Eye Contact Lens. 2021:1-6. |


