 |
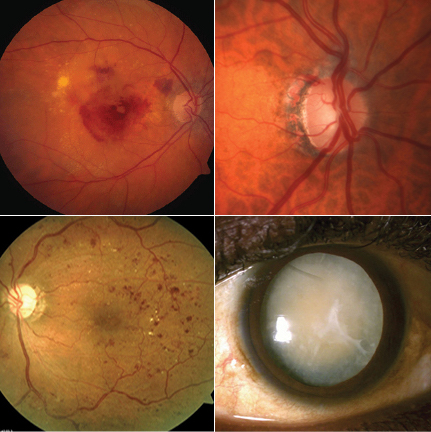
| Of 30 million Medicare beneficiaries in this study, 41% had at least one claim for either AMD, glaucoma, cataract or diabetic retinopathy. Click image to enlarge. |
The latest report on the impact of age-related eye diseases (AMD, glaucoma, cataract and diabetic retinopathy) on the Medicare burden says that a significant portion of patients are affected by these diseases and that related spending accounts for approximately 4.3% of Medicare Part B and 1% of Medicare Part D spending. Overall, vision loss and eye disorders cost an estimated $139 billion in 2013.
“New estimates of the burden of these conditions to Medicare are warranted by the advent of new treatment, increased aging of the United States population, changes in Medicare’s reimbursement policies and changes in the proportion of Medicare enrollees enrolled in FFS,” the researchers explained. “Additionally, the analysis of 100% of the Medicare FFS data allows for a full accounting of costs and reporting by detailed demographic groups and by state.”
To determine the proportion of beneficiaries who had at least one claim indicating AMD, cataract, DR or glaucoma, and their payments, the researchers analyzed Medicare Part B FFS claims and Part D Events. Beneficiaries included in the study were continuously enrolled in Medicare for 12 months in 2018. The researchers used the CDC definitions of the diseases to identify cases and reported outcomes overall and by age, sex, race and ethnicity and US state.
They gathered data from approximately 30 million beneficiaries, and more than 41% (12.4 million) of these patients had at least one claim for one of the four age-related eye diseases. Payments totaled $10.1 billion ($3.6 billion for cataract, $3.5 billion for AMD, $2.2 billion for glaucoma and $0.8 billion for DR). Average cost per beneficiary was $816 ($1,290 for AMD, $781 for DR, $543 for glaucoma and $360 for cataract).
“AMD, glaucoma, DR and cataract together are sometimes referred to as the ‘big four’ of eye diseases as they’re believed to cause the majority of vision loss and blindness in the US,” the researchers said. “We find that together these conditions were diagnosed in over 41% (12.4 million) of Medicare FFS beneficiaries in 2018, and were responsible for $10.1 billion in annual direct payments, including $2.5 billion in out-of-pocket payments. Medicare Part B payments for the four conditions totaled $9.1 billion, which constituted over 4% of total Medicare Part B payments in 2018. Payments for glaucoma drugs under Part D were $948 million, which was 1% of the total costs for Medicare Part D in 2018. This analysis doesn’t include beneficiaries enrolled in Medicare MA plans, which if included, would increase the number of beneficiaries by 52%.”
The researchers say that overall costs have increased over the past decade, but the costs associated with the four eye diseases have varied, including decreased spending toward cataracts (-34%), which previously cost more than the other three diseases combined. “This decrease was more than offset by increases in the costs of the other three conditions, including a 500% increase for AMD and a 230% increase in DR costs,” they noted. “The underlying causes of these dramatic changes in payments for each disease are likely complex but may include changes in cataract surgery reimbursement, the emergence of costly anti-VEGF therapies for AMD and DR and coverage of glaucoma prescriptions under Medicare Part D.”
The researchers concluded that these four conditions have major consequences for Medicare, since more than 40% of beneficiaries are affected. “Continued increases in the number and age of Medicare beneficiaries may be expected to contribute to future growth in these costs to the Medicare program.”
Wittenborn JS, Gu Q, Erdem E, et al. The prevalence of diagnosis of major eye diseases and their associated payments in the Medicare Fee-for-Service Program. Ophthalmic Epidemiol September 16, 2021. [Epub ahead of print]. |


