 |
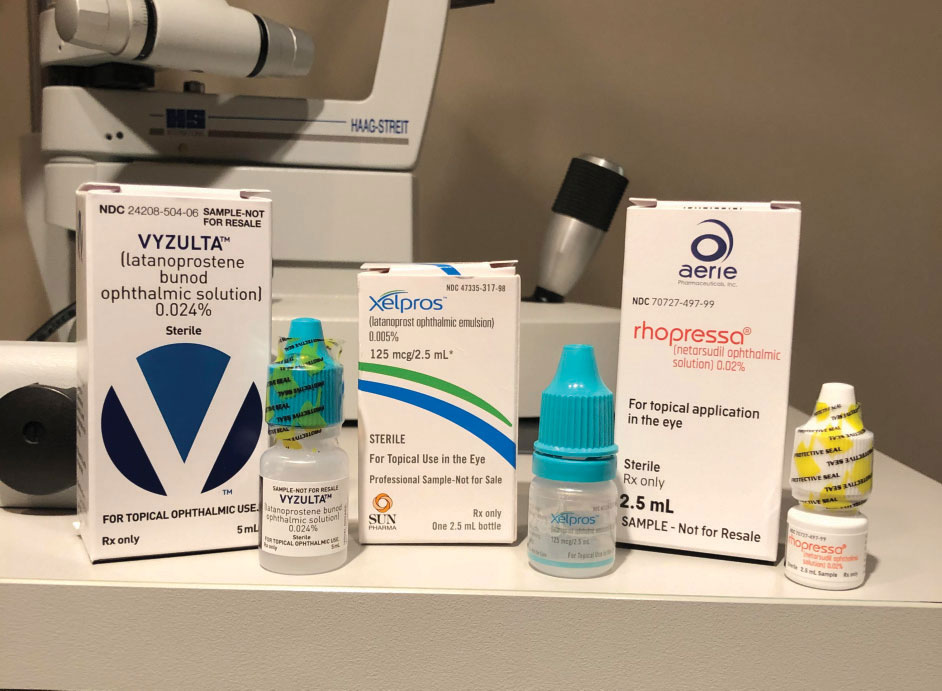
| Patients with certain disabilities may be more likely to struggle with glaucoma medication compliance. Photo: Greg Caldwell, OD, Tracy Offerdahl, PharmD, and Joseph Sowka, OD. Click image to enlarge. |
ODs face a perennial challenge in trying to make sure their glaucoma patients stay current with their medications, but a new study reports another wrinkle in this effort: certain types of disabilities can reduce medication compliance by about 18%. Specifically, the investigators found patients who have limb disability, are in a vegetative state or have dementia attended up to three fewer outpatient visits and had lower medication adherence (between 0.7% and 17.6%).
“In this study, we found that glaucoma medication adherence increased or decreased depending on the type of disability. However, overall, glaucoma outpatient visits and medication adherence were higher among people with disability,” the authors wrote in their paper.
The population-based, case-control study enrolled individuals with glaucoma but without a disability who were followed until they received disability certification. All patients in Taiwan with confirmed glaucoma in one or both eyes were identified using the National Health Insurance claims database. All patients with glaucoma (confirmed glaucoma, suspected glaucoma and ocular hypertension) who required medication and had newly obtained disability status after December 2013 were identified and matched to counterparts without disability based on age and sex. The study period ran from 1997 to 2017, and total enrollment included roughly 46,5000 patients with glaucoma (about 23,200 with a disability and 23,200 without a disability).
Key study highlights included:
The frequency of glaucoma outpatient visits was higher in people with disabilities compared with those without disabilities both before and after the index dates when using one-year intervals. However, when stratified by disability type, limb disability, being in a vegetative state and dementia were linked with fewer outpatient visits and lower medication adherence compared with individuals without a disability.
Adjusted regression results revealed that people with visual disability had approximately 2.50-times more glaucoma outpatient visits vs. those who were disability-free.
“We found that people with visual disability had higher glaucoma medication adherence,” the authors said. “In Taiwan, people who qualify for a visual disability status are not necessarily completely blind. This may explain why greater effort was made by these patients to ensure the maintenance of their vision.”
This finding contrasts with a Singaporean study, which reported that people with visual impairment had low eye care utilization, they added. The discrepancy is likely attributable to different definitions for visual disability and visual impairment in their study, researchers explained.
Although lack of eye care can lead to visual impairment, the study adds to existing knowledge, since people with visual impairment may not have had lower eye care utilization prior to the impairment than their counterparts who are disability-free, the authors said. However, this higher level of use may not necessarily prevent them from developing visual disability, they added. Additionally, eye care utilization increases after visual disability, leading to a higher burden for both the individual and the economy, but these patients continue to have suboptimal outcomes, the researchers suggested.
The study results recommend that policies targeting glaucoma medication adherence consider disability types, the authors concluded.
Ho CH, Pu C. Medication adherence in patients with glaucoma and disability. JAMA Ophthalmol. October 28, 2021. [Epub ahead of print]. |


