In April 2016, optometry lost a giant when the author of the seminal work Primary Care of the Posterior Segment, Larry Alexander, OD, died. In addition to being an optometric physician, author and educator at the University of Alabama Birmingham School of Optometry, Dr. Alexander was a past president of the Optometric Retina Society (ORS). That group chose to honor his legacy by accepting case reports from optometric residents across the country relating to vitreoretinal disease.
The two cases shown here, selected by the ORS Awards Committee, were co-winners of the sixth annual Larry Alexander Resident Case Report Contest. The contest is sponsored by Topcon, Visionix (Optovue) and Heidelberg.
“When reviewing submissions, we look for manuscripts that are well written, include high-quality images and provide new and innovative information to the community,” says Julie Rodman, OD, professor and chief of the Fort Lauderdale (Broward) Eye Care Institute at Nova Southeastern University in Florida, and ORS treasurer. “This year, our winning manuscripts focused on timely topics and provided insight into the diagnosis and management of entities that are often challenging to diagnose,” she notes.
The full text and images of both case reports are available online at the links below.
Case #1: Bilateral Bartonella henselae Neuroretinitis
Claire Cordoba, OD, a primary care resident at the Indiana University School of Optometry, presented a case of an 18-year-old with severe bilateral neuroretinitis caused by Bartonella henselae, which causes 22,000 cases of cat scratch disease globally per year. She noted that ocular involvement occurs in 5-10% of affected patients and typically presents two to three weeks after systemic symptoms begin. The report discussed which examinations to perform to ensure a proper diagnosis, as well as explained the various clinical characteristics of the condition including associated ocular signs and symptoms.
 |
|
Right eye with 4+ optic nerve head edema with overlying granuloma, cystoid macular edema and myelinated retinal nerve fiber layer with possible retinitis. Click image to enlarge. |
Among Dr. Cordoba’s conclusions from the case was that multiple differentials need to be considered when Bartonella is suspected in a patient, including HIV, HZV/HSV, leptospirosis, Lyme, syphilis, toxocariasis, toxoplasmosis and tuberculosis. She also emphasized the importance of early blood testing to test for Bartonella antibodies, which helps to identify the cause of the infection and begin treatment sooner to avoid potentially devastating visual outcomes.
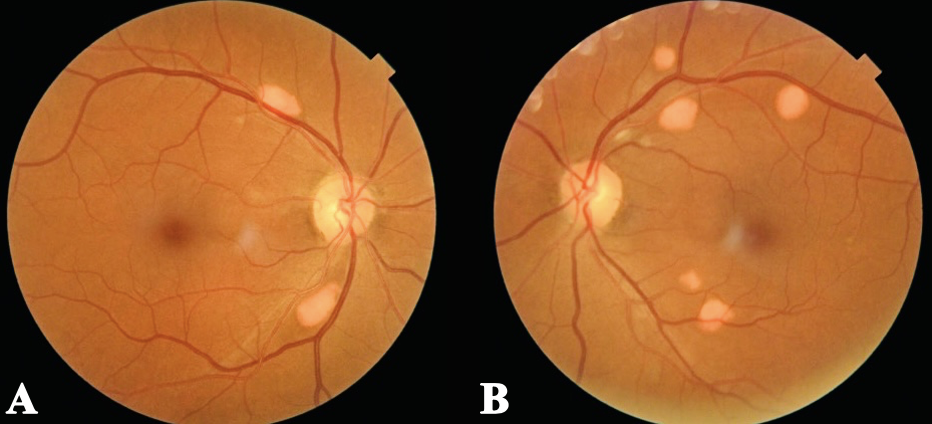
Case #2: Multifocal Vitelliform Dystrophy
This case report by Keying Yan, OD, ocular disease optometry resident at the BronxCare Health System in New York, discusses a rare condition called multifocal vitelliform dystrophy (MVD), presenting as multiple yellow vitelliform lesions in the subretinal space. The case features a 67-year-old male with MVD who had asymptomatic but chronic, progressive lesions and describes the diagnosis, treatment and management of the disease.
 |
|
Fundus photos of both eyes (right eye: A; left eye: B) show scattered elevated, orange-yellow lesions with distinct borders, located along the superotemporal and inferotemporal retinal vascular arcades within the posterior pole. Click image to enlarge. |
MVD can be either familial or sporadic, and the pathophysiology for multifocal vitelliform lesions remains unknown. Dr. Yan noted that in some cases, MVD is associated with BEST1 gene variation, referred to as multifocal Best disease. The report also noted that “lesions in patients without the genetic mutation tend to be smaller in size and higher in numbers.” Though no treatment currently exists for MVD, Dr. Yan concludes that affected patients should be regularly monitored for potential secondary complications that may require referral to a retinal specialist. In addition, she highlights the important role of research that can provide insight on the condition’s etiology and identify effective management techniques.


