The fairly common posterior segment finding of retinoschisis—prevalence ranges from 7% to 22% in the literature—can sometimes be mistaken for a retinal detachment, leading to concerns about misdiagnosis that may not be warranted.
One recent study employed various color and autofluorescence imaging modalities obtained with a scanning laser ophthalmoscope (California or Silverstone, both from Optos) as well as peripheral OCT images (from the Silverstone device) to identify features of the degenerative condition. Such devices use red and green lasers to generate a “pseudocolor” image of the retina as well as red- and green-separated photos, which may be better suited to specific purposes. For instance, the Toronto-based researchers explain in their paper for Acta Ophthalmologica that the green-separated image provides a detailed depiction of neurosensory retina down to RPE, while the red-separated image provides a view from the RPE down to the choroid.
 |
|
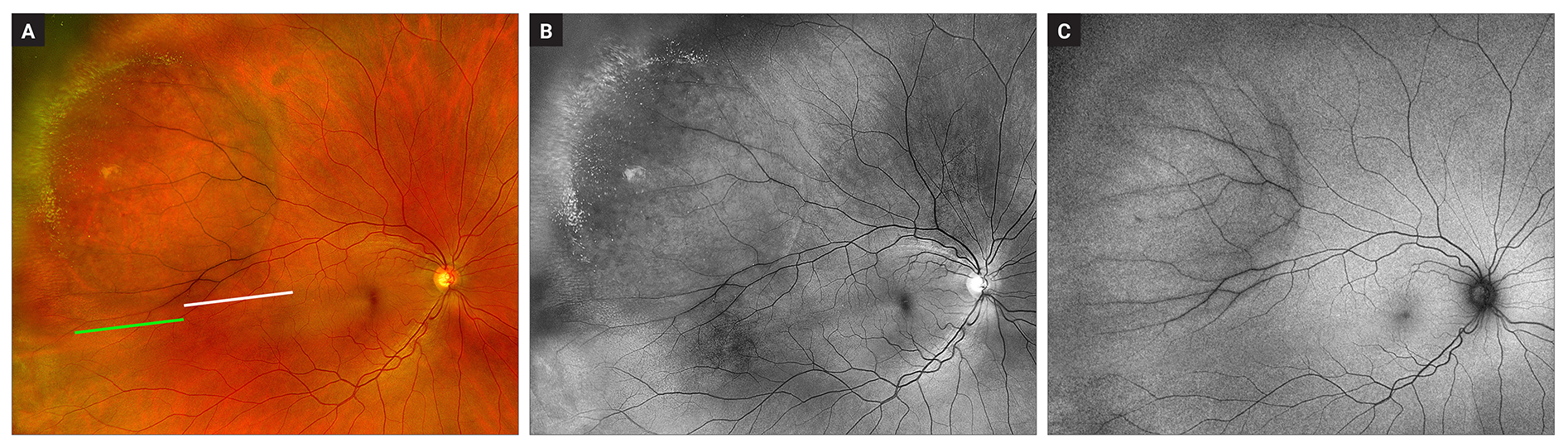
These images from the study show superotemporal degenerative retinoschisis in the right eye: (a) Pseudocolor image shows smooth, dome-shaped retinal elevation with well-defined and darker vasculature. Reticular pattern is visible in the anterior half of the area of retinoschisis and there are hyperreflective foci present at the anterior border of the area of retinoschisis. (b) Green-separated image showing reticular pattern and hyperreflective foci corresponding to the distribution on the pseudocolor image. (c) Autofluorescence imaging showing a hypoautofluorescent posterior border and isoautofluorescence over the area of schisis. Photo: Orr S, et al. Acta Ophthalmol. March 27, 2024. Click image to enlarge. |
Included in the retrospective investigation were 139 total eyes. The researchers found a hyporeflective reticular pattern associated with retinoschisis on pseudocolor images in 39% of cases; this percentage increased in visibility of 53% on green-separated images. Almost half (49%) of cases were observed to have hyperreflective foci. Finally, retinoschisis was confirmed with OCT in 27% of eyes.
Upon further discussion, the study authors add that most cases (80%) were inferotemporal, which aligns with previous literature reports. They also observed that many eyes had schisis in more than one quadrant—with 60% of eyes displaying superotemporal retinoschisis, which is much higher than previous studies accounting 28%. There were also less bilateral cases than seen in prior research (50% vs. 77%). However, they authors point out this difference may be due to this practice’s comprehensive imaging protocols, potentially detecting subtle degenerative retinoschisis signs earlier.
Isoautofluoresence (uniformity in signal intensity between affected and unaffected tissue) is most commonly characteristic of retinoschisis, occurring in around 68% to 100% of cases in literature, either with or without a hypoautofluorescent posterior border. This cohort fell within this range, representing 80% that were isoautofluorescent over the area of schisis. As well, a hypoautofluorescent posterior border of retinoschisis was seen in 35% of this cohort, similar to previous reports of 30% to 33%.
Perhaps most interesting are the pseudocolor imaging findings of this study. On this type of imaging, retinoschisis has been described as a smooth, dome-shaped elevation without folds or undulations. As well, vessels can appear dark over the schisis area, which is likely an imaging artifact caused by retinal elevation. The current study expands upon pseudocolor image findings—described in this cohort were instances of a reticular pattern and bright, hyperreflective foci, neither of which have been previously discussed.
The researchers believe that “this reticular pattern is likely representative of schisis cavities in the neurosensory retina,” they wrote. As such, they analyzed the green-separated images, since they can provide more information about this structure; this led to an even more prominent pattern seen on these images. Some cases did not display the pattern on pseudocolor imaging but did with green-separated images. The pattern was visible on green-separated images in 73 eyes; of those, only 74% showed the pattern on pseudocolor imaging.
As for the yellowish-green foci, the authors explain these may represent glial dots. The hyperreflective foci’s prominence on green-separated images but subtle or absent appearance on red-separated images led the authors to believe the pathology is located within the neurosensory retina. This observation aligns with the hypothesis that the foci represent glial cell remnants.
Taking these points into consideration, the authors conclude that “these findings may denote the presence of otherwise subtle retinoschisis, aid in differentiation from RD and inform management decisions.”
Orr S, Hatamnejad A, Sodhi S, et al. Novel features of degenerative retinoschisis identified using ultra-widefield multicolor channels. Acta Ophthalmol. March 27, 2024. [Epub ahead of print]. |


