 |
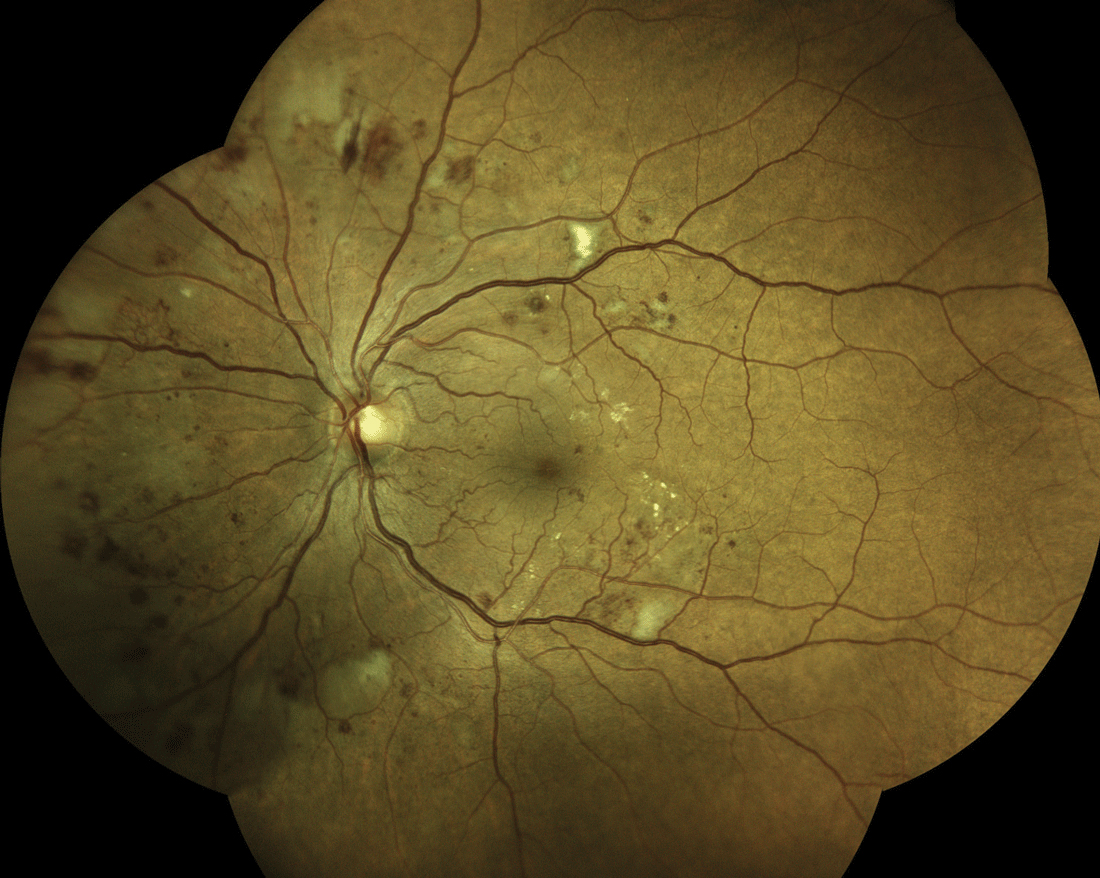
| When monitoring patients with diabetic retinopathy, consider the type of medication they’re on and their current retinopathy status to help guide treatment decisions, as this study found that medication class can influence progression to PDR or new-onset DME. Click image to enlarge. |
In the past few years, the FDA has approved several novel hypoglycemic medications, such as GLP-1 agonists or SGLT-2 inhibitors, indicated for patients with diabetes to help improve glucose control, consequently helping stave off disease-related complications like diabetic retinopathy (DR). While keeping blood sugars in range reduces long-term risks of microvascular complications in diabetes mellitus, research is conflicting regarding the specific effects of these popular new drugs on DR progression. To investigate, the authors of a new clinical cohort study evaluated the effects of both GLP-1 agonists and SGLT-2 inhibitors on DR and its progression using a large, diverse, real-world population database. Their findings, described below, were recently published in American Journal of Ophthalmology.
Included patients had an ICD-10 code of non-proliferative DR (NPDR) and monotherapy treatment, excluding insulin, with GLP-1 agonists or SGLT-2 inhibitors. Those with a history of PDR were excluded. The researchers compared the rate of progression to PDR and rate of development of diabetic macular edema between patients on GLP-1 agonists vs. those on SGLT-2 inhibitors. After propensity score matching, a total of 6,481 patients were identified in each medication group.
The results showed that patients on monotherapy with GLP-1 agonists had a higher rate of progression to PDR compared to those on SGLT-2 inhibitors, demonstrated at year one and year three after initiation of therapy. The GLP-1 agonist group also had a higher rate of new-onset DME than the SGLT-2 inhibitor group, observable at multiple time points, including three months, six months, one year and three years after initiation of therapy. Importantly, the researchers also pointed out in their paper, “This class-specific difference in developing vision-threatening complications appeared to be more pronounced over time.”
There was no significant difference in mean HbA1c levels or the need for secondary interventions such as intravitreal anti-VEGF injections, panretinal laser photocoagulation or pars plana vitrectomy between the GLP-1 agonist group and the SGLT-2 inhibitor group, except for a slightly higher need for anti-VEGF agents in the GLP-1 agonist group at three years.
The researchers concluded, “Our large retrospective cohort study found that GLP-1 agonists carried a higher rate of progression to PDR and DME compared to SGLT-2 inhibitors.” They encouraged clinicians “to be aware of these potential effects and to consider the current retinopathy status when initiating treatment with newer hypoglycemic agents to ensure these patients are appropriately monitored for developing potential vision-threatening complications.”
Wai KM, Mishra K, Koo E, et al. Impact of GLP-1 Agonists and SGLT-2 inhibitors on diabetic retinopathy progression: an aggregated electronic health record data study. Lee et al. Am J Ophthalmol. April 2024. [Epub ahead of print]. |


