| |
|
|
| Vol. 22, #20 • Monday, May 24, 2021 |
|
| |
|
Off the Cuff: A New Way to Assess Your Success in Managing Dry Eye
Of all things, a good clinician must be focused on outcomes. While that would seem a self-evident truth, the noise, marketing mumbo-jumbo and fast-pace of contemporary practice can obscure what really counts most—how your patient actually feels. In other words, did you make them better or not? If you ask most patients, feeling, seeing or looking better is what is important to them and, like it or not, that’s how they judge how effective you are.
A while back I had an epiphany. After looking over a patient’s improved SPEED score and getting a positive status update from my tech Donna, who had just finished working them up, I realized that I was walking into the exam room already thinking that I had missed something or hadn’t done enough to address their issues. That feeling persisted even after the patient confirmed how well they were doing as I was already pondering what I needed to do next.
I finally traced my whacky behavior to having a judgmental father for whom even 100% wasn’t good enough and my natural compulsive need to solve problems. For those of you who are thinking, poor guy, he had a terrible childhood, actually my judgmental dad did an incredible job preparing me for life and especially for clinical practice. As a clinician, I am never completely satisfied and always striving to be better. As a speaker and educator, good is never good enough. Never buying my own “PR” keeps me humble.
I know. You are wondering what childhood neurosis and questionable parenting skills have to do with dry eye. Actually, quite a bit. Realizing that always feeling like I had to fix something when nothing was broken wasn’t particularly productive, so I came up with a workaround. I found a simple way to quantify the patient’s success and, in turn, my clinical success along with it.
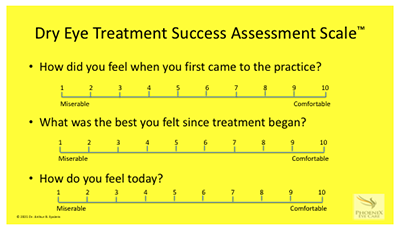
The Dry Eye Treatment Success Assessment Scale™ or the Epstein Dry Eye Treatment Success Assessment Scale™ as I force everyone in the office to call it, is a simple three-question verbal analog scale that captures: 1) how the patient felt when they first came to see me, 2) how they felt when they felt the best since beginning treatment and 3) how they feel today. I don’t actually fill out the scale; the graphic below is to help you get the picture, but in about 30 seconds it definitively tells me that there is either more work to be done or reminds patients of how much progress we’ve made. The latter is almost always the case.
 |
At some point I will likely validate the DETSAS™ and publish it in a refereed journal, but I find it so useful that I wanted to share it with as many of you as possible as quickly as possible. Feel free to use it and please let me know if you find it helpful or if you have any suggestions. One other thing my father taught me is to always welcome helpful advice.
Want to share your perspective?
Write to Dr. Epstein at artepstein@optometricphysician.com.
The views expressed in this editorial are solely those of the author and do not necessarily represent the opinions of Jobson Medical Information LLC (JMI), or any other entities or individuals.
|
|
|
|
|
| |
|
A Widefield Optical Coherence Tomography Normative Database Considering the Fovea-disc Relationship for Glaucoma Detection
One purpose of this study was to collect widefield swept-source optical coherence tomography (SS-OCT) data from healthy eyes and build a wide-filed normative database. Another purpose was to compare the glaucoma diagnostic ability of new parameters based on this normative database to the parameters that are currently in use, such as the peripapillary retinal nerve fiber layer (RNFL), macular ganglion cell-inner plexiform layer and ganglion cell complex (GCC) thickness. This study had 220 healthy eyes and 292 eyes with early-stage glaucoma (EG) and moderate-stage glaucoma (MG) enrolled. Using the widefield SS-OCT images (12 × 9mm) of healthy eyes, a widefield normative database was constructed by transforming and combining the individual images into a uniform template using the fovea and optic disc centers as fixed landmarks. Adjustment for the disc size was conducted. With this normative database, new parameters based on the ratio of the fovea-disc distance (FDD) consisting of the fovea-disc relationship were evaluated. The glaucoma diagnostic ability was assessed based on the area under the receiver operating characteristic curve (AUC).
Among the new peripapillary parameters, the RNFL of the circumference of the circle with diameter 0.8 FDD showed the highest AUC value for EG and MG, but the value was not significantly superior to that of the initial RNFL (AUC=0.940 vs. 0.937, p=0.631). Among the macular parameters, the GCC of the area of the circle of 1.5 FDD showed the highest AUC value for EG and MG, and the value was significantly superior to that of initial GCC (AUC=0.929 vs. 0.919, p=0.033). However, there was no significant difference between the initial and adjusted GCC thickness in patients included in the EG or MG groups separately.
A widefield normative database was built to consider the relationship between the fovea and the optic disc. Researchers found that the GCC analysis using a broader area presented a significantly greater glaucoma diagnostic performance for EG and MG in the macula than the initial parameter for the GCC.
SOURCE: Kim H, Lee JS, Park HM, et al. A Wide-field optical coherence tomography normative database considering the fovea-disc relationship for glaucoma detection. Transl Vis Sci Technol. 2021; Feb 5;10(2):7.
|
|
|
|
|
|
|
|
| |
|
Longitudinal Development of Refractive Error in Children Treated With Intravitreal Bevacizumab or Laser for Retinopathy of Prematurity
This study compared the patterns of longitudinal refractive error development during the first 3.5 years in children with severe retinopathy of prematurity (ROP) treated with intravitreal bevacizumab (IVB) or laser photocoagulation. This prospective cohort study enrolled extremely preterm infants (birth weight <1000 g, gestational age 23 to 27 weeks) with type 1 ROP from multiple hospitals in Dallas between 1999 and 2017; IVB group (n=22); laser group (n=26). Cycloplegic retinoscopy was conducted from 0.04 years corrected age and every 0.5 to 1.0 years thereafter until 3.5 years old. Right eye spherical equivalent (SEQ) and astigmatism, anisometropia and better-eye visual acuity were analyzed over time.
In all children, both eyes were treated with the same modality. At the final visit, the prevalence of myopia (SEQ ≤ -1D) was 82.7% in the laser group and 47.7% in the IVB group with a mean SEQ of -8.0D ± 5.8D in the laser group vs. -2.3D ± 4.2D in the IVB group. Longitudinal SEQ were best fit with a bilinear model. Before one year, the rate of SEQ change was -5.0D/year in the laser group, but only -3.5D/year in the IVB group; after one year, there was a significant flattening of these slopes. Anisometropia in the IVB group was significantly less than in the laser group. Final visual acuity in both groups was similar at 0.47 logMAR (∼20/60).
Children with severe ROP treated with IVB developed less myopic refractive error than those treated with laser largely because of a slower rate of refractive change during the first year of life.
SOURCE: Simmons M, Wang J, Leffler JN, et al. Longitudinal development of refractive error in children treated with intravitreal bevacizumab or laser for retinopathy of prematurity. Transl Vis Sci Technol. 2021l Apr 1;10(4):14.
|
|
|
|
|
| |
| |
|
Change in Refractive Error Associated with the Use of Cannabidiol Oil
Cannabinoid (CBD) products have gained popularity since their legalization in 2018, causing a plethora of unregulated CBD products to be sold in the United States. These products are available in various combinations for topical and oral consumption, claiming credit for potentially improving various diseases. In this report, we present a newfound case reporting a shift in refraction that may be associated with the regular use of CBD oil supplements.
A 57-year-old woman with a history of diabetes mellitus type 2, hyperlipidemia, obstructive sleep apnea, with no change in medications, diet or lifestyle was found to have a hyperopic shift in vision with the recent daily addition of CBD oil intake. This case report highlighted the possible association of CBD oil and vision changes after regular consumption of CBD oil in an otherwise stable patient. Further study is required to understand the mechanisms of CBD oil-associated shift in refractive error. Because the patient was diabetic and the refraction shift was hyperopic, other etiologies, such as un-noted lenticular change, cannot be ruled out.
The authors wrote that CBD products are unregulated and marketed in many mixed forms, and thus can cause unforeseen effects on susceptible individuals. They suggested that FDA regulation of such products and extensive research is warranted before considering them for therapeutic usage.
SOURCE: Ali A, Gupta PK. Change in Refractive Error Associated With the Use of Cannabidiol Oil. Cureus. 2021 Apr 12;13(4):e14434.
|
|
|
|
|
|
|
|
|
|
Industry News
Review's New Technologies & Treatments Meeting Goes High Tech and All Virtual in June
With many doctors still wanting the flexibility to attend meetings virtually, Review Group today announced an enhanced all-virtual event, New Technologies & Treatments (NT&T) in Eye Care Summer 2021 conference, offering an interactive format and numerous opportunities for attendees to gain clinical pearls and knowledge in areas critical to their practice. The Review Group includes Review of Optometry, Review of Ophthalmology, Review of Cornea and Contact Lenses and Retina Specialist. Published by Jobson Healthcare Information, the journals provide the latest clinical insight and education to optometrists and ophthalmologists. Scheduled for June 11 to 12, the conference will feature "Grand Rounds in Retina, Glaucoma and Anterior Segment Disease," and additional talks on glaucoma, retinal disease and ocular surface disease, especially in the area of new pharmaceutical agents and technologies. The conference will be chaired by Paul Karpecki, OD, FAAO, chief clinical editor for Review of Optometry, clinical director, Corneal Services and Advanced Ocular Surface Disease at Kentucky Eye Institute and a clinician for Gaddie Eye Centers. Read more.
Essilor Receives FDA Breakthrough Device Designation for Stellest Lens in Myopia Efforts
Essilor announced the FDA granted Breakthrough Device designation to its Stellest spectacle lens to correct myopia and slow down the progression of myopia in children. The designation comes after the publication of two-year results of an ongoing three-year clinical trial in myopic children in China. After the first year, the trial results demonstrated that the eye growth of nine out of 10 children wearing the Essilor Stellest lens was similar or slower than non-myopic children. Read more.
New Study Identifies Number of People with Vision Loss and Blindness
In a study published in JAMA Ophthalmology titled “Prevalence of Visual Acuity Loss or Blindness in the US,” researchers estimate more than 7 million people are living with uncorrectable vision loss, including more than 1 million Americans who are living with blindness. The study was authored by researchers from the Institute for Health Metrics and Evaluation at the University of Washington, NORC at the University of Chicago, and the Centers for Disease Control and Prevention’s Vision Health Initiative, with support from Prevent Blindness. Read more.
Study Finds ImprimisRx’s Klarity-C Drops Safe and Effective
ImprimisRx announced a study of its Klarity-C Drops (cyclosporine 0.1% ophthalmic emulsion PF) published in Clinical Ophthalmology concluded that dry eye treatment with twice daily cyclosporine 0.1% in chondroitin sulfate emulsion was found to be safe and effective in reducing signs and symptoms of dry eye. Read more.
Heru Funding Accelerates Cloud & AI-enabled Wearable Vision Diagnosis & Therapy
Heru closed its Series A financing of $30 million to advance the company’s eye diagnostic and vision correction technology platform. The company continues to collaborate with developers of next-generation augmented reality headsets for compatibility with off-the-shelf AR/VR headsets such including Microsoft and Magic Leap devices, and is developing vision augmentation software designed to correct the user’s vision defects in real time using AI. Read more.
|
|
|
|
|
Optometric Physician™ (OP) newsletter is owned and published by Dr. Arthur Epstein. It is distributed by the Review Group, a Division of Jobson Medical Information LLC (JMI), 19 Campus Boulevard, Newtown Square, PA 19073.
To change your email address, reply to this email. Write "change of address" in the subject line. Make sure to provide us with your old and new address.
To ensure delivery, please be sure to add Optometricphysician@jobsonmail.com to your address book or safe senders list.
Click here if you do not want to receive future emails from Optometric Physician.
HOW TO SUBMIT NEWS
E-mail optometricphysician@jobson.com or FAX your news to: 610.492.1039.
Advertising: For information on advertising in this e-mail newsletter, please contact sales managers Michael Hoster, Michele Barrett or Jonathan Dardine.
News: To submit news or contact the editor, send an e-mail, or FAX your news to 610.492.1049
|
|
|
|
|
|
|
|
|