
From the Desk of The President
 I am excited to present our second newsletter. Our last issue discussed preoperative issues. This newsletter focuses on post-operative topics like medications, treatments and patient satisfaction. The OCCRS is working to increase comanagement among optometrists, and awareness about the latest news in our industry.
I am excited to present our second newsletter. Our last issue discussed preoperative issues. This newsletter focuses on post-operative topics like medications, treatments and patient satisfaction. The OCCRS is working to increase comanagement among optometrists, and awareness about the latest news in our industry.
Some of our members spend every day in the comanagement world working alongside our surgical partners. Others are in optometric offices practicing to the fullest extent of their state laws. It is the mission of OCCRS to educate doctors about modern corneal, cataract or refractive procedures to deliver the highest level of care to their patients in whatever practice modality they enjoy.
If you are interested in membership, including the private listserve, go to www.OCCRS.ORG to learn more.
I hope you enjoy this issue and look forward to our quarterly updates.
Tracy Schroeder Swartz, OD, MS, FAAO, Dipl ABO,
President, OCCRS
Annual Meeting

We are already planning for the 2020 Annual Symposium. This two-day event showcases the latest in technology for corneal, cataract and refractive procedures, and updates attendees on present and future comanagement information. More information will be available on our public Facebook page, as well as our website: www.OCCRS.org
![]()
Cornea, Cataract and Refractive Surgery Management
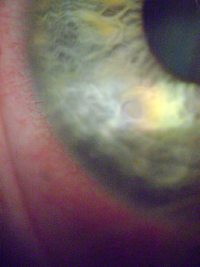
Corneal abrasion with associated inflammation (courtesy of Tracy S. Swartz, OD, MS)
Inflammation and OSD After Surgery
Last spring, eye care suffered a critical shortage of prednisolone acetate. For approximately six weeks, the drug was unavailable. Suddenly, we had to decide what steroids to use after phacoemulsification and keratorefractive surgeries. While patients with commercial insurance could use pharmaceutical company discount programs, our Medicare patients could not. This led many providers to reconsider their postoperative drop regime.
The purpose of antibiotic and anti-inflammatory drops after surgery is to prevent infection and control inflammation. We polled the OCCRS listserve to see what our doctors were doing during this shortage. Most reported ordering combination drops containing Pred acetate, or prescribing generic flurometholone, and loteprednol and difluprednate when affordable. During this time, I added an extra postoperative visit to ensure inflammation was controlled. Since risk factors for persistent iritis after cataract surgery include patients who are diabetic or African American, and use of a pupil expansion device during surgery1, I followed these patients more closely.
Talk regarding steroid- or NSAID-only versus steroid/NSAID combinations after surgery also increased, as cost is a factor for our elderly patients. Controversy continues as to what postoperative drop regime is better. In fact, a review of 48 studies of drop regimes after cataract surgery found insufficient evidence to inform practice for treatment of postoperative inflammation after uncomplicated phacoemulsification.2
With any ocular surgery, the exacerbation of ocular surface disease is also a concern. Corneal incisions disrupt the feedback loop between the lacrimal gland and corneal nerves. Intraoperative actions such as prolonged exposure to the microscope light, aggressive irrigation and frequent topical anesthetic drops traumatize the corneal epithelium and/or conjunctival mucous goblet cells. Frequent use of drops with preservatives and an overall increase in inflammation will increase symptoms. Diligence during the postoperative period to optimize each patient’s treatment is critical to ensure patient satisfaction.
1. Neatrour K, McAlpine A, Owens TB, et al. Evaluation of the etiology of persistent iritis after cataract surgery. J Ophthalmic Inflamm Infect. 2019 Feb 18;9(1):4. doi: 10.1186/s12348-019-0170-2.
2.
Juthani VV, Clearfield E, Chuck RS. Non-steroidal anti-inflammatory drugs versus corticosteroids for controlling inflammation after uncomplicated cataract surgery. Cochrane Database of Systematic Reviews. 2017 Jul 3;7: CD010516. DOI: 10.1002/14651858.CD010516.pub2
![]()
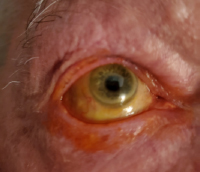
Severe lid disease in an 75-year-old, previously untreated patient. (Courtesy of Tracy S. Swartz, OD, MS)
Modern Topical Lid Treatments: Not Your Mother’s Baby Shampoo
If lid disease increases after ocular surgery, your patient will likely complain that the surgery “made their eyes worse,” even if the surgery technically went perfectly. While lid hygiene may be the best treatment, compliance is an issue when patients have been using drops for four weeks already. Patients with subjective symptoms are more likely to continue therapy long-term compared to those with clinical signs but no subjective discomfort. Specialty lid formulations better address lid disease than baby shampoo or OTC lid scrubs. These include tea tree oil, hypocholorous acid, Abelmoschus esculentus (okra) and topical steroids.
Tea tree oil targets Demodex, the mite commonly found in the lashes of elderly patients. Several topical preparations have been used to cure demodex infections. Gao, et al. reported that 10% povidone-iodine, 75% alcohol, 50% baby shampoo and 4% pilocarpine failed to kill Demodex after extended exposure, while survival time was limited to 15 minutes in 100% alcohol, 100% TTO, 100% caraway oil or 100% dill weed oil. The same author also evaluated efficacy of tea tree oil scrubs in 11 patients with ocular Demodex who received weekly lid scrub with 50% TTO combined with daily lid hygiene with tea tree shampoo. After TTO lid scrub, the Demodex count dropped to zero for two consecutive visits in less than four weeks, in eight of 11 patients. This is important to note for our patients desiring resolution of symptoms after surgery. Read More.

Patient Satisfaction After Surgery
Research shows that patient satisfaction after surgery is related more to visual outcome and subjective improvement than clinical outcome. How many times have you seen a patient whose surgery went perfectly, and yet, they are upset with their results? A perfect surgical outcome does not guarantee a happy patient. This is particularly true in patients with a low level of health literacy, and the presence of systemic and ocular comorbidity.
One cross-sectional study evaluated 150 patients 50 years and older who had their first eye’s cataract surgery using a written questionnaire. Researchers found patient satisfaction with hospital care had a stronger correlation with overall satisfaction than patient satisfaction with the medical outcome (r=0.669 versus r=0.543, respectively). They concluded satisfaction was more related to the patient's preoperative expectations and the quality of care given perioperatively. Read more.
