Modern cataract surgery is extremely safe, but the sheer volume of procedures performed—roughly four million each year in the US alone—means that adverse events will affect a sizable number of people. As the intraoperative complication of posterior capsular rupture (PCR) can negatively impact final visual outcome for patients, researchers and clinicians alike would like to know what risk factors are present for PCR during cataract surgery.
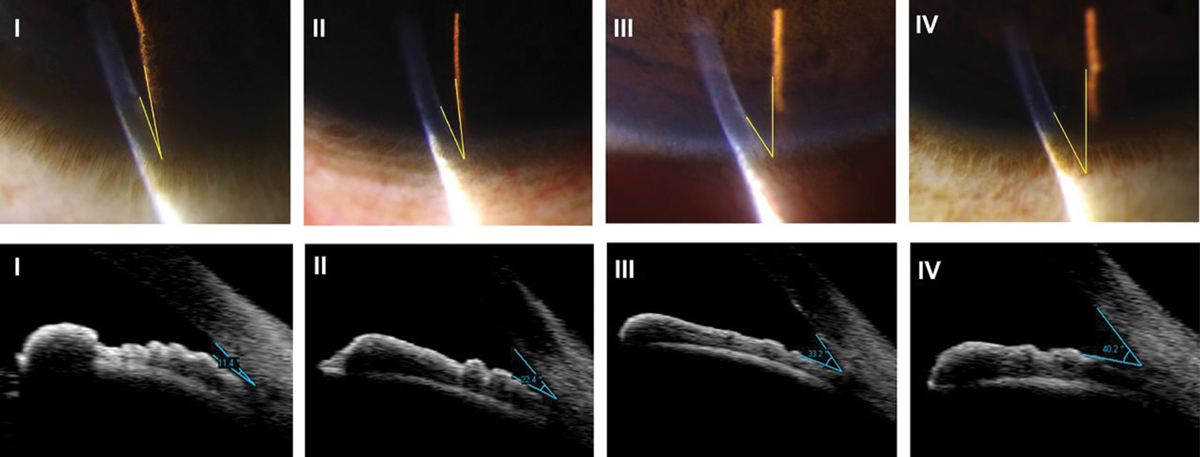 |
| A shallow anterior chamber depth of <2.2mm was associated with increased PCR rates, possibly due to iris prolapse being more common, thus surgeons making longer tunnels and increasing corneal distortion and impairing visualization, or more directly increasing proximity of instruments to the posterior capsule in a shallow anterior chamber. Shown here is the Van Herick grading stages. Photo: Amila Herbert, OD. Click image to enlarge. |
Included in a new investigation were eligible operations from centers supplying data to the UK national cataract audit with complete data, including patients’ sex, age at surgery, anterior chamber depth and preoperative visual acuity. A model was designed to identify risk factors and calculated the odds ratios of factors on PCR likelihood. Results were published last week in the British journal Eye.
A significant 961,208 cataract operations were included, performed on 682,381 patients from 136 different centers and with 3,198 different surgeons. Only 1.01% of these surgeries had PCR occur, with a median age of 75.7 for the first eye surgery and 76.7 for the second among affected patients. Of those who had PCR occur, 53.0% were women. The highest risk factors for PCR included less experienced trainee surgeon, pseudoexfoliation/phacodonesis, younger men and brunescent/white/mature cataract. Other identified risk factors were glaucoma, worse preoperative visual acuity, previous intravitreal therapy, high myopia, previous vitrectomy, systemic diabetes, diabetic retinopathy, amblyopia, older age, shallower anterior chamber depth and an inability to lie flat at cooperate.
As part of their discussion, the study authors relay that these findings confirmed previously known risk factors of increasing age, trainee surgeon, male sex, inability to lie flat and cooperate, systemic diabetes, diabetic retinopathy, smaller pupil size, mature cataract, glaucoma and pseudoexfoliation/phacodonesis, with corroboration of more recently reported risk factors, too, of previous intravitreal anti-VEGF therapy and worse preoperative visual acuity. What’s more interesting are the novel risk factors identified of high myopia, previous vitrectomy, shallow anterior chamber depth and amblyopia.
They elaborate more on individual risk factors, stating that one of the highest odds ratios was in younger men; however, they note that the age/sex interaction term diminished this ratio in older patients, with similar risk in sexes by age 85, and even a switch of women having greater risk after 90 years of age.
The authors theorize that the novel risk factor of high myopia might affect PCR by a longer axial length making surgery more challenging, but previous literature hasn’t found association between axial length specifically and PCR, thus suggesting other mechanisms at play, like higher cataract density.
Those who had a pervious vitrectomy may have had higher PCR risk due to altered fluid dynamics, unstable posterior capsules or posterior lenticular touch during vitrectomy, with the underlying increased PCR risk in these eyes potentially overlapping with high myopia, since the two possess a strong correlation.
Generally, the authors convey that “this analysis provides an update to the current risk adjustment model for PCR with the quantification of additional risk factors.”
As they explain, this information “will facilitate a bespoke, contemporary risk assessment tailored to an individual patient’s operation, thereby allowing more informed patient counseling, appropriate case allocation and adoption of precautionary measures to minimize the risk of PCR during surgery.”
| Click here for journal source. |
Sim PY, Donachie PHJ, Day AC, Buchan JC. The Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: a risk factor model for posterior capsule rupture. Eye (Lond). September 19, 2024. [Epub ahead of print]. |


