A 72-year-old white female initially presented in October 2000, and was diagnosed
with normotensive glaucoma (NTG). She later moved to Alaska, but eventually returned to the area. Meantime, she stopped using her medication.

Now, 18 months after her initial visit, her current findings suggest that a subtle progression may have occurred, although her visual fields did not change.
Diagnostic Data
When I initially saw her in October 2000, a full glaucoma work-up indicated the early presence of glaucomatous optic neuropathy in both eyes, O.S.>O.D. Her entering pressures prior to initiating therapy were (on average) 19mm Hg O.U.
Cup-to-disc ratios were 0.45x0.50 O.D. and 0.55x0.70 O.S. There was a small pigment crescent adjacent to the right nerve and a mild peripapillary atrophy in the left eye. Threshold visual field studies demonstrated scattered paracentral scotomas O.S.>O.D.; these were consistent with the areas of thinned neuroretinal rim.
She began therapy with Timoptic-XE 0.50% (timolol maleate) 1 gtt O.U. q a.m., which lowered IOP to the mid-teen range.
A few months later, the patient moved to Alaska for about nine months. While there, she discontinued her medication.
When she moved back to the area, I saw her again in early April 2002. Her unmedicated IOPs were 20mm Hg O.D. and 21mm Hg O.S. Her anterior and posterior segments were unremarkable, except for mild nuclear sclerosis O.U. Gonioscopy demonstrated grade II open angles with a mild amount of trabecular pigmentation O.U.
Through dilated pupils, her C/D ratio appeared the same as one year earlier. The neuroretinal rim in the left eye was thinned inferotemporally, as before. I compared previous digital images using the Eyescape Digital Imaging System; there appeared to be no appreciable difference in optic nerve appearance in either eye.
However, there was an increase in the extent of the peripapillary atrophy (PPA) in the left eye, specifically in the zone beta component of the PPA. Threshold fields, however, demonstrated no significant change in mean deviation, pattern standard deviation or corrected pattern standard deviation over time.
I restarted her on medication, but this time I chose Lumigan (bimatoprost), 1 gtt O.U. hs. In my experience, we are more likely to lower IOPs with monotherapy using a prostaglandin. She is due back in two months for re-evaluation.
Discussion
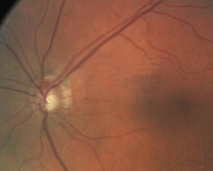
Current retinal photo shows the extent of zone beta peripapillary atrophy O.S.
When we manage glaucoma patients, we often tend to concentrate on IOP, visual fields and neuroretinal rim characteristics, and ignore other important indicators of glaucomatous progression. One such indicator that clinicians often overlook is peripapillary atrophy.
PPA refers to the atrophic-like changes that occur to the retina and choroid immediately adjacent to the optic nerve. Generally, there are two types, based on location and appearance:
Zone beta is usually located closest to the nerve. Loss of the underlying RPE and choroid in a visible scleral crescent characterizes this form of PPA. It results in an absolute scotoma.1
Zone alpha is located circumferentially further away from the nerve. Pigmentary disruption of the RPE characterizes zone alpha PPA. Doctors sometimes refer to it as the chorio-pigment epithelio-retinal atrophy (a pigmentary disruption of the RPE and choroid). It results in a relative scotoma.1
How does PPA suggest the progression of glaucomatous optic neuropathy? Studies indicate several important facts about PPA. First, both glaucomatous visual field loss and the area of neuroretinal rim tissue loss are consistent and greatest in the areas of zone beta.2-5 The correlation between neuroretinal rim loss and visual field progression is not significant when compared with zone alpha.2,3 Although there can be significant variations in the appearance of PPA when viewed at different times and by different observers, zone beta seems to be the most reproducible of the characteristics of PPA, which makes it a good marker in clinical practice.6
However, there appear to be different mechanisms involved in the development of PPA in patients with open-angle glaucoma and angle-closure glaucoma.7 So, monitoring zone beta PPA in open-angle glaucoma is more reliable than it is in other forms of glaucoma.
Zone beta PPA can also be a predictor in differentiating normotensive glaucoma from glaucoma suspect nerves. One study found that the area of zone beta was statistically larger in patients with normotensive glaucoma when compared with matched patients (age, IOP, C/D ratio) who did not have visual field loss.8 Another study found a strong correlation between the progression of PPA, visual field loss and thinning of the neuroretinal rim.9 Earlier studies also showed that as PPA progresses, so too does glaucomatous damage.10
This brings us back to the patient in this case. Although her visual fields have remained stable, and her neuroretinal rim also appears stable, her zone beta PPA clearly increased. Two recent studies (preceded by several other studies), strongly imply that not only does PPA progress along with nerve and field loss in open-angle normotensive patients, but it may also precede such damagea good indicator of the likelihood of glaucoma progression.4,8,10
In short, look not only at visual fields, IOP and neuroretinal rims, but also very closely at peripapillary atrophy.
1. Jonas JB, Gusek GC, Fernandez MC. Correlation of the blind spot size to the area of the optic disc and peripapillary atrophy. Am J Ophthalmol 1991 May 15;112(5):609.
2. Park KH, Tomita G, et al. Correlation between peripapillary atrophy and optic nerve damage in normal tension glaucoma. Ophthalmology 1996 Nov.;103(11):1899-906.
3. Jonas JB, Naumann GO. Parapapillary region in normal and glaucoma eyes. II. Correlation of planimetric findings in intrapapillary, perimetry and general data. Klin Monatsbl Augenheilkd 1988 Aug; 193(2):182-8.
4. Law SK, Choe R, Caprioli J. Optic disk characteristics before the occurrence of disk hemorrhage in glaucoma patients. Am J Ophthalmol 2001 Sept;132(3):411-3.
5. Daugeliene L, Yamamoto T, Kitazawa Y. Risk factors for visual field damage progression in normal-tension glaucoma eyes. Graefes Arch Clin Exp Ophthalmol 1999 Feb;237(2):105-8.
6. Tuulonen A, Jonas JB, et al. Interobserver variation in the measurements of peripapillary atrophy in glaucoma. Ophthalmology 1996 Mar;103(3):535-41.
7. Uchida H, et al. Peripapillary atrophy in primary angle-closure glaucoma: a comparative study with primary open-angle glaucoma. Am J Ophthalmol 1999 Feb;127(2):121-8.
8. Park KH, Park SJ, et al. Ability of peripapillary parameters to differentiate normal-tension glaucoma from glaucoma-like disk. J Glaucoma 2001 Apr;10(2):95-101.
9. Uchida H, Ugurlu S, Caprioli J. Increasing peripapillary atrophy is associated with progressive glaucoma. Ophthalmology 1998 Aug;105(8):1541-5.
10. Uhm KB, Lee DY, et al. Peripapillary atrophy in normal and primary open angle glaucoma. Korean J Ophthalmol 1998 June;12(1):37-50.

