
Cornea, Cataract and Refractive Surgery Management
Is the Eye Ready for Surgery?
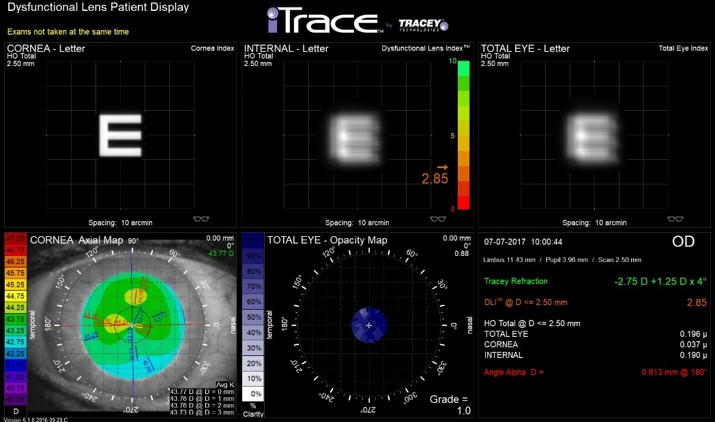
Figure 1. This iTrace display (Tracey Technologies, Houston, TX) demonstrates the effect of the healthy external cornea (clear, left “E”), cataractous lens (blurry, middle “E”) and overall vision (blurry right “E”). This patient’s blurry vision is due to the cataract, and this patient is read for surgery.
Images: Tracy Schroeder Swartz, OD, MS, FAAO, Dipl ABO
Patients’ options for vision correction have advanced considerably. Not only do we have wavefront-guided and wavefront-optimized LASIK, we now have topography-integrated as well as topography-guided applications. These require higher order aberrations and topography information to be acquired for surgical planning. Ocular surface disease can affect these measurements and, subsequently, the outcomes.
Cataract surgery also requires corneal measurements. Biometry, or axial length measurement, is now performed optically rather than with ultrasound. Autokeratometry or topography used in intraocular lens (IOL) calculations is critical for strong outcomes and also may be influenced by ocular surface disease.
It is important to consider whether the patient you are referring for surgery is ready for these measurements. Treating ocular inflammation, lid disease including meibomian gland dysfunction and blepharitis, and corneal issues prior to referral ensures correct measurements and demonstrates clinical prowess to the surgeon. Consider addressing corneal issues such as EBMD, Salzmann’s degeneration or keratoconus prior to cataract surgery. This may be accomplished by referring to a corneal specialist for both corneal and cataract evaluation, or may require separate referrals.
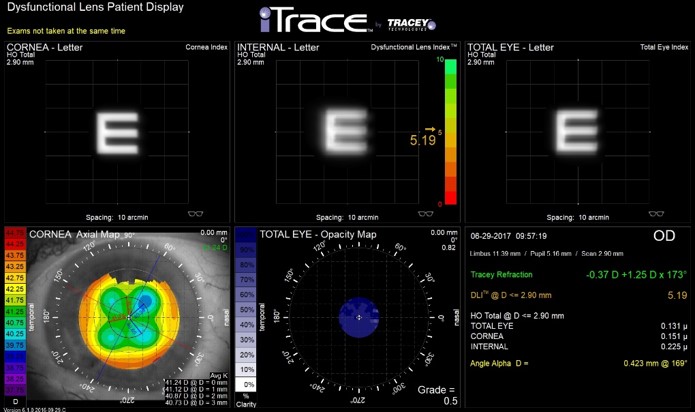
Figure 2. Note the topographical pattern of Radial Keratotomy (RK) in the lower left map. Treatment of the ocular surface is recommended in all patients post-refractive surgery to maximize the measurements. These calculations are problematic, and refractive surprises may be minimized with pretreatment and extensive patient education.
An unhealthy ocular surface affects IOL calculations, toric IOL axis and magnitude estimates, keratometry, topography measurements, and increases surgical difficulty.i Treating severe ocular surface disease after the procedure is less effective in reducing the patient’s anxiety about their outcome. Patient-reported visual functioning, dry eye symptoms, and health anxiety are more closely associated with patients' postoperative satisfaction than with objective clinical measures of visual acuity or signs of dry eye.ii
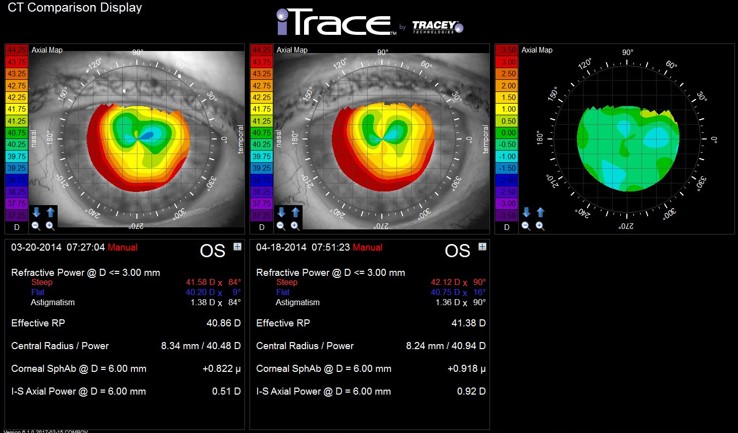
Figure 3. Note the change in Effective Refractive Power (ERP) from 40.86D to 41.38D after one month of treatment. The steep meridian increased from 41.58D to 42.12D. When assessing topography, one should examine the pattern as well as indices and keratometry values. If significant change is noted at one month, further treatment and repeated topography may be indicated.
When examining a patient for cataract surgery, consider the tear film, examine the lids and assess the ocular surface using topography. (Figure 1) Patients with a history of refractive surgery should be treated for at least one month prior to surgery for best results. (Figure 2) If treatment is indicated, initiate your course of therapy. Upon return, reassess topography for a change in curvature. Demonstrate the effect for the patient in order to reassure them the treatment is working, and this will improve their final outcome.
Treatment of significant ocular surface disease may change the corneal power. Figure 3 demonstrates the change in Effective Refractive Power (ERP) from 40.86D to 41.38D after one month of treatment. The steep meridian increased from 41.58D to 42.12D. If significant change is noted at one month, further treatment and repeated topography may be indicated. Figure 4 demonstrates a change of 2.35D after three months of treatment.
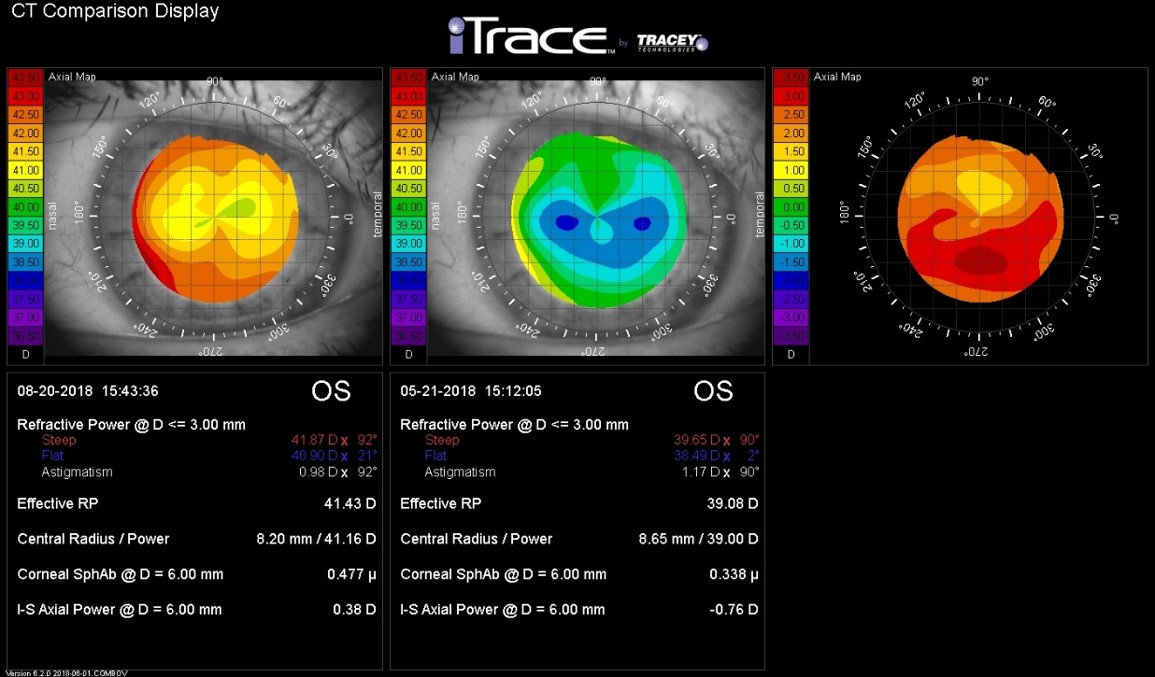
Figure 4. This patient was followed for three months prior to surgery. Note treatment resulted in a change of 2.35D after three months of treatment. The inferior steepening found in May resolved with treatment.
Once the ocular surface is stabilized, the patient will be more reassured about their decision to proceed with surgery. Postoperative management should include assessment of any ocular surface disease, which is likely to increase after surgery. That topic is for our next newsletter.
i Chuang J, Shih KC, Chan TC, et al. Preoperative optimization of ocular surface disease before cataract surgery. J Cataract Refract Surg. 2017 Dec;43(12):1596-1607. doi: 10.1016/j.jcrs.2017.10.033.
ii Szakáts I, Sebestyén M, Tóth É, et al. Dry eye symptoms, patient-reported visual functioning, and health anxiety influencing patient satisfaction after cataract surgery. Curr Eye Res. 2017 Jun;42(6):832-836. doi: 10.1080/02713683.2016.1262429. Epub 2017 Jan 27.
