 |
A 24-year-old student at an optometry college was participating in the retinal examination laboratory. She had a history of trauma to the left eye. She explained that, as a child, she had taken a fall that resulted in an eye injury. She had not required hospitalization and reported that the injury was treated supportively.
She had no known allergies and denied a history of systemic disease or medications of any kind.
Her best-corrected entering visual acuity through -6.50D spectacles was 20/20 O.U. at distance and near. Her external examination was normal. There was no afferent pupillary defect, and refraction was stable with negligible changes. Biomicroscopic examination revealed normal and healthy structures in both eyes. Goldmann applanation tonometry measured intraocular pressure of 17mm Hg O.U.
The important posterior segment finding in her left eye is demonstrated in the photograph.
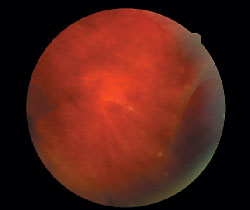 |
| The patients retinal appearance in her left eye. |
Your Diagnosis
How would you approach this case? Does this patient require additional tests? What is your diagnosis? How would you manage this patient? What is the likely prognosis?
Discussion
Additional testing included scleral depression of the lesion, three-mirror Goldmann retinal evaluation of the left eye and Optos Optomap photodocumentation.
The diagnosis in this case is a retinal tear with subretinal fluid and shallow rhegmatogenous retinal detachment (RRD), O.S. RRD is defined as a separation of the neurosensory retina from the retinal pigment epithelium secondary to a seepage of fluid from the vitreous humor through a full-thickness retinal break.1-6
Patients who present with RRD often describe the characteristic symptom of photopsia.1 The photopsia phenomenon resolves when adhesions surrounding the retinal tear become released.
Floaters, another common symptom of RRD, present in three forms:1
Solitary, or ring-shaped (secondary to posterior vitreous detachment from the margin of optic disc).
A sudden shower of multiple floaters (usually secondary to vitreous hemorrhage from a damaged peripheral vessel at the time of a tear).
Strands that appear as cobwebs (condensation within collapsed vitreous).
RRD may also occur with a visual field defect, perceived as a dark curtain located in the area of the primary detachment.1
In non-traumatic RRD, the most common etiology is secondary to lattice degeneration (LD).2 LD appears in early life and stabilizes during the second decade.3 It is most often found in myopic eyes and located between 11 and 1 o"clock or between 5 and 7 o"clock.3 Atrophic holes within areas of lattice frequently cause retinal detachment when liquefied vitreous fluid passes through the break and into the subretinal space.3
While approximately 30% of RRDs result from lattice degeneration, research on the natural history of the condition suggests that prophylactic treatment of lattice lesions is not necessarily indicated.4-6 Prophylactic treatment is indicated when patients present with high myopia, a history of retinal detachment in the same eye or fellow eye, cataract extraction, a family history of retinal detachment or a history of conditions that predispose them to retinal detachments such as Marfan"s syndrome, Stickler"s syndrome and Ehlers-Danlos syndrome.4
Prophylactic treatment of RRD may be dispensed using one of three treatment modalities: slit-lamp laser photocoagulation; cryotherapy; or indirect ophthalmoscopic laser photocoagulation. Choice of modality depends on the location of the RRD and personal preference of the doctor.
Advanced treatment modalities for RRD include scleral buckling and pneumatic retinopexy. Scleral buckling involves indentation of the sclera in an effort to close the offending tear(s) and reduce traction.1 It is often performed in cases of large U-shaped (horseshoe) tears, wide dialyses and multiple breaks involving one or two quadrants.1
Pneumatic retinopexy involves injection of intravitreal gas to seal the retinal break. It can be accomplished with or without the need for buckling. This procedure is indicated in a small break or a small cluster of breaks that extend less than two clock hours in the superior two-thirds of the peripheral retina.1
The prognosis of RRD depends on the extent of detachment, type of treatment, involvement of the macula and treatment modality employed to repair it.
The patient in this case required surgical intervention with barrier laser photocoagulation, which was completed without complications. Follow-up visits have demonstrated a good repair.
1. Kanski J. Retinal Detachment. In: Kanski J. Clinical Ophthalmology: A Systemic Approach. 5th ed. Philadelphia: Butterworth-Heinemann, 2003:348-388.
2. Kaiser F. Retina and Choroid. In: Kaiser F. The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. 2nd ed. Philadelphia: Saunders, 1998:289-423.
3. Lewis H. Peripheral retinal degenerations and the risk of retinal detachment. Am J Ophthalmol 2003 Jul;136(1):155-60.
4. Byer NE. Long-term natural history of lattice degeneration of the retina. Ophthalmology 1989 Sep;96(9):1396-401.
5. Wilkinson CP. Evidence-based analysis of prophylactic treatment of asymptomatic retinal breaks and lattice degeneration. Ophthalmology 2000 Jan;107(1):12-5.
6. Avitabile T, Bonfiglio V, Reibaldi M, et al. Prophylactic treatment of the fellow eye of patients with retinal detachment: a retrospective study. Graefes Arch Clin Exp Ophthalmol 2004 Mar;242(3):191-6.
Thanks to Virginia Donati, B.Sc., for contributing to this case.

