Pediatric optometry offers the opportunity to experience, to paraphrase Charles Dickens, “the best of times and the worst of times.” For the most part, the good outweighs the bad.
A pediatric optometrist can rest easy knowing she is working to change children’s lives by correcting their refractive errors, combating amblyopia and even diagnosing early cases of disease such as retinoblastoma—getting a jump on not only saving the eye but, potentially, a child’s life. These experiences can be tremendously rewarding.
However, the “worst of times” include dealing with patients who scream and cry when simple drops are administered (something adult-oriented optometrists rarely encounter), negotiating undisciplined children (and parents) and, most seriously, discovering diagnoses with troubling implications such as bilateral retinal hemorrhages, which are often secondary to child abuse.
With the advent of the Affordable Care Act (ACA), predictions project an increase of pediatric patients in general practices. According AOA past president David Cockrell, OD, “we all need to become more proficient in pediatric eye care.”
This article offers a glimpse into the world of pediatric optometry and what it takes to incorporate this rewarding specialty.
Why Should You be Interested in Pediatrics?
Pediatric patients historically have been underserved. For years, federal agencies and school systems have communicated that a vision screening qualifies as a comprehensive examination by an eye care provider. Nothing could be further from the truth. Optometrists know that vision screenings are not enough to fully reveal undetected vision problems such as amblyopia, latent refractive error, systemic diseases and learning disorders, many of which vision therapy can help remedy. Undetected vision problems require a complete workup and, often, comanagement subsequent to their detection.
It was one of the greatest legislative achievements of our day to have the pediatric comprehensive eye exam (not simply a screening) included in the 10 essential health benefits defined in the law. Now, millions of children in the United States have access to comprehensive ophthalmic examinations, and optometrists have the chance to make history because of our unique ability to provide these greatly needed services.
 |
| Getting kids to sit still is a trick of the trade. One solution: ask them to hold on to a little friend, like this young lady and her elephant. It can help soothe anxieties and keep tiny hands busy. |
Adding pediatric services also opens other doors the ACA affords optometry. For one, offering advanced pediatric eye care is smart business. Practices must continue to find ways to diversify their revenue stream to maintain profitability. The medical pediatric model presents a significant opportunity for eye care professionals.
Typically a pediatric patient takes less time than an adult and, with proper scheduling, a clinician can see an increase in gross revenue per month. Another advantage is that families can come in together and have their examinations at the same time, therefore grouping the exams closer and adding more patients per day. Furthermore, by adding pediatric management to your optical, you can outpace competition with a wider frame selection and increased expertise.
An Optical Shop for the Younger Crop
In general practices, most frames are adult sized. Pediatric optometrists must be fiercely intentional about supplying the optical with the necessary sizes and brands—not to mention the staff training to ensure service and profitability.
Many optical frame brands address the pediatric population’s specific needs. Lightweight frames are especially vital for pediatric patients, as standard polycarbonate lenses that are +4.00 or greater are thick and heavy on the bridges of tiny noses. Further complicating higher prescriptions, both myopic and hyperopic, is weight and cosmetic effect, which can be remedied by high index or aspheric lens designs. Miraflex and other brands offer frames with a bridge built to accommodate a flatter nose, which most children have. Every optical should be armed with proper staff training in pediatric frame adjustments and additional accessories such as Stayputs—slip on, adjustable devices that fit onto the back surface of the frame temple.
The impact of a proper lens prescription on a child’s life is immeasurable. Take, for example, the case of an eight-year-old Hispanic female who presented to my office with uncorrected visual acuities of 20/80 OD and 20/60 OS. She had fallen behind in school, according to her grandfather. Her cycloplegic refraction was +3.00-4.00x180 OD, and +2.00-3.75x180 OS.
She had bilateral refractive amblyopia and was best corrected to 20/40 OU.
After every pediatric exam, I tell my young patients that I saw their brain and that their brain is very smart. After I recited the line to this particular patient, her eyes welled up with tears. That’s when I found out that her classmates had called her “dumb.” I told her she was not dumb, but that she was very smart and that her glasses would help her move to the top of the class.
After two months with her prescribed glasses, she returned with 20/25 OU vision, along with a bright smile on her face and a glowing report from her grandfather, who boasted that she’d advanced from being the last in her class to one of the top three.
Being a pediatric optometrist gives you the opportunity to change not only the sight of a child, but change the course of their lives.
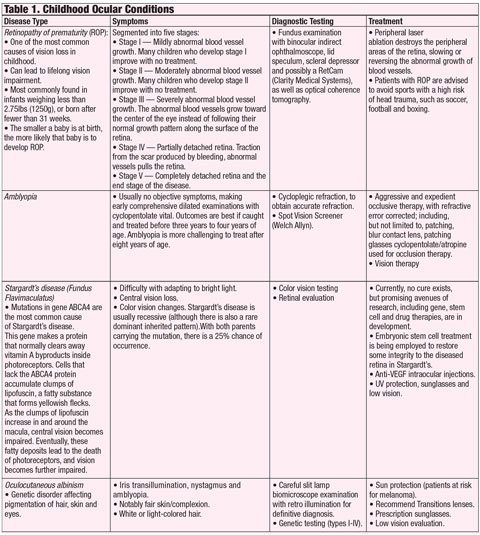 |
| Click chart to enlarge. Click here to download PDF. |
The Medical Model for Kids
Primarily, children see an OD to address a refractive error, like in the above encounter. But, like adults, children sometimes develop eye diseases and you may end up saving their vision, or even their life.
Ten years ago, I was doing a routine dilated exam on a six-year-old male patient—incidentally, the patient was my nephew. He was plano in both eyes, had passed the school screening and the pediatric vision screening. However, upon dilation, I noticed a two-disc diameter fleshy tumor of the optic nerve in his right eye. After three trips to three different pediatric retinal specialists, his scans were sent to Wills Eye Institute in Philadelphia, where Jerry Shields, MD, confirmed a diagnosis of active retinoblastoma. We were fortunate, as within two weeks, the tumor had outgrown its blood supply and had become calcific tissue.
Today, he is a healthy teenage boy who still checks in with a retina specialist once every five years. This was a close call, but the potential consequences of overlooking this diagnosis could have been dire.
 |
| To be a successful pediatric OD, get familiar with products specific to this clientele, such as this device that prevents frames from slipping. |
Although this isn’t a common condition, some diseases are more common in children (Table 1). For example, pediatric optometrists must always be on the prowl for amblyopia, which must be caught and treated before age eight to 10 to prevent permanent visual impairment; ideally, for the best outcome it needs to be caught by age three. Aggressive occlusive and vision therapy, as well as accurate refraction ascertained from a cycloplegic refraction, are needed to ensure amblyopia is prevented.
Comanagement
Comanagement allows optometry to develop a good working relationship with pediatric ophthalmology and other interdisciplinary avenues of care, such as pediatricians, pediatric neurologists, nurses, PAs, endocrinologists and geneticists.
Pediatricians and family practice doctors benefit immensely from comanagement with optometry. These doctors aren’t always comfortable treating pediatric ocular issues. For example, without a slit lamp, it’s difficult to properly diagnose the etiology of a red eye, or remove a foreign body. In regards to a red eye, most default to a broad-spectrum antibiotic, which will not be effective if the cause is viral or the result of an allergic condition, and in regards to a foreign body, most pediatricians, nurses, or PAs are not trained in how to properly remove a foreign body. It behooves you to reach out to other specialties to offer your eye care expertise.
One tool in particular has been a game changer in early diagnosis and treatment of amblyopia and refractive error: the Spot Vision Screener (Welch Allyn). We encourage general and pediatric medical clinics to incorporate this technology in every pediatric exam, regardless of age. Amblyopia can be detected even in newborns by a novice health care worker with this technology.
As optometry develops greater comfort in pediatric care, comanagement doors will open wider for the benefit of the patient and provider.
Challenges in the Chair
Now for the bad news: children can wreak havoc upon an office. Children often touch and maneuver equipment, in spite of posted warning signs. Frustrating as it is, unruliness is natural in children.
 |
| Remember to invite pediatric patients in by preparing not only your exam lane, but your waiting area as well. |
But combating unruliness in parents is the real challenge. A certain percentage of parents will actually push back against instilling eye drops in the child’s eyes, claiming it burns. In those cases, properly educate the parent that the precision of the refraction and the accuracy of the health diagnosis depends on the cycloplegic dilated eye exam.
Whether pediatric patients struggle with attention deficit disorders or not, visiting the optometrist isn’t exactly a day at the park. Children can quickly grow impatient and begin to squirm. Here is a pearl I often use: as soon as a child sits down, give him a toy to play with. Next, raise the chair, place the phoropter in front of his eyes with the cartoons used for acuity testing preloaded onto the eye chart. I can then perform retinoscopy. If the child tries to reach up and touch the dials, remind him to keep his hands down and hang on to the toy. Smaller children will have retinoscopy performed with lens bars. I usually give children a toy in the shape of an animal, and we proceed to examine the toy’s eyes—afterwards, children are often more accommodating and will allow you to perform the BIO, slit lamp and further testing . It also helps to have young children sit in their parent’s lap so you can do a demonstration on the parent. This can help allay children’s fears and make them more accommodating. Be sure to apply 1% cyclopentolate and 2.5% phenylephrine 45 minutes before the exam so the child is completely cyclopleged.
Let Your Office Reflect Your ExpertiseIf you’re considering focusing on a pediatric patient base, obtain the proper education to do so. But one thing you might not learn in your CE courses is how to present the proper office aesthetic. Here are some updates to consider: 1. Make your office more kid friendly by including toys and games in the exam room and dedicating a corner of your waiting area to kids. 2. Consider designing a pediatric exam room. Include a Snellen chart with cartoons and lens bars, and brush up on your skills on retinoscopy with lens bars. 3. Invest in equipment that is germane to the pediatric population: a portable slit lamp, a kid-friendly tonometer such as the Icare brand and amblyopic materials such as eyepatches and brochures explaining strabismus and amblyopia. You can use the resources provided by the AOA to immediately position your practice as a pediatric optometric practice. “Think about your eyes,” and “Infant See” are public health initiatives to educate parents seeking an optometrist to provide care for their children. |
If a child is uncooperative on the visual acuity, retinoscope or BIO, we perform a partial exam, prescribe the cyclopentolate 1% and 2.5% phenylephrine to the parent and have them return another day with the child already dilated. We instruct the parent to put the drops in one hour before the appointment. The parent is instructed on proper drop installation and dosage before they leave the office.
You can also incorporate a reward system, with parental approval, where pediatric patients are offered a toy from a “treasure box” or piece of candy after the exam, if they can maintain proper behavior.
There’s never been a better time to enter the world of pediatrics, and optometry is primed to take the lead in managing this patient group. One in four children has an undiagnosed vision problem, leading to everything from chronic headaches to difficulty in school or trouble reading.1 Make sure to protect children’s vision health by adding a pediatric comprehensive eye exam to your list of services.
Dr. Elliott is the optometric director of a high volume pediatric ophthalmology practice in Tulsa, OK, cofounder of www.take10vision.com and a continuing education speaker.
| 1. Kleinstein R, Jones L, Hullett S, et al. Refractive error and ethnicity in children. Arch Ophthalmol 2003;121:1141-7. |

