 |
Best-corrected visual acuity at this exam was 20/70 in the left eye. Confrontation fields in that eye were full to careful finger counting. The left pupil was round and reactive to light, and the anterior segment exam was unremarkable. Her prosthetic right eye fit well and appeared to have excellent cosmesis with her left eye.
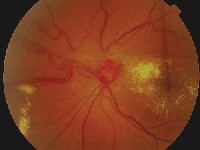 |
| 1. Dilated fundus exam revealed exudates in the macula and dilated vessels that extended nasally from the optic nerve. |
 |
| 2. On the fluorescein angiogram, the angioma appears adjacent to the optic nerve. |
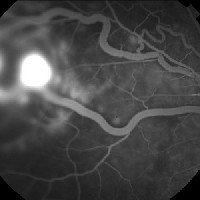 |
| 3. The angioma hyperfluoresces almost immediately, and we can see the peripheral angioma begin to light up. |
1. What is the significance of the dilated retinal vessels that extend from the optic nerve?
a. Congenital dilated vessels.
b. Arteriovenous malformation.
c. Afferent/efferent vessels.
d. Pending central retinal vein occlusion (CRVO).
2. The dilated retinal vessels suggest what type of lesion involving the optic nerve?
a. Cavernous hemangioma.
b. Retinal capillary hemangioma (RCH).
c. Retinal angioma.
d. Both b and c.
3. What is the correct diagnosis for this condition?
a. Von Hippel tumor.
b. Pending CRVO.
c. Wyburn-Mason syndrome.
d. Coats disease.
4. What is the most significant complication associated with this patients diagnosis?
a. Tumor of the central nervous system (CNS).
b. Stroke secondary to arteriovenous malformation.
c. Neovascular glaucoma.
d. Cystoid macular edema.
5. What additional testing should be done?
a. Magnetic resonance imaging.
b. Blood pressure check.
c. Carotid studies.
d. Chest X-ray.
6. How should this patient be treated?
a. Observation.
b. Laser photocoagulation.
c. External beam radiation.
d. Eye wall resection.
For answers, go to bottom of page.
Discussion
A vascular lesion adjacent to the optic nerve superiorly is leaking exudates into the macula. This lesion represents a juxtapapillary endophytic capillary hemangioma of the retina, otherwise known as a von Hippel tumor.
A second tumor is located nasally in the mid-peripheral retina. An obvious clue: the dilated artery and vein that extend nasally from the nerve. The artery and vein represent the afferent feeder and efferent drainage vessels that lead to this second RCH (figure 2).
A third tumor is present superior nasally. However, this is much smaller than the others and resembles nothing more than a large non-conspicuous microaneurysm.
On fluorescein angiography, the angioma appears adjacent to the optic nerve (figure 2). It hyperfluoresces almost immediately, and we can see the peripheral angioma begin to light up (figure 3). The peripheral lesion may have an additional smaller angioma that was not appreciated clinically.
Capillary hemangiomas are angiomatous hamartomas of the retina that are pathognomonic of von Hippel disease. These hemangiomas can present as a peripheral lesion with a definite afferent and efferent vascular system or as a juxtapapillary tumor.
They also can present as an endophytic mass that projects into the vitreous or an exophytic mass that extends toward the outer retina. These types of masses tend to be flatter and grayer in color, and they do not have the afferent feeder vessel. Endophytic tumors appear as fleshy red vascular masses that are typically round or have a bulb-like configuration. Our patient has both the peripheral tumor and the lesion adjacent to the nerve. Both are endophytic in nature.
An RCH begins as a small red dot that sometimes resembles the microaneurysms seen in early diabetic retinopathy. Our patient has a supertemporal RCH.
As these tumors enlarge, they begin to leak exudative material. If this occurs near the macula, vision loss can develop due to macular edema. Also, larger peripheral tumors can develop exudative retinal detachments that may be very difficult to manage. Our patient underwent enucleation of her right eye 25 years ago due to a complicated exudative retinal detachmentthe result of an RCH.
The presence of any RCH within the eye suggests possible systemic disease. These hemangiomas are commonly associated with CNS hemangioblastomas and visceral carcinomas, including renal cell carcinoma and pheochromocytomas.1
German ophthalmologist Eugen von Hippel (1867-1939) first described the isolate RCH in 1926. Arvid Lindau (1892-1958), a Swedish pathologist, discovered the association of RCH and CNS tumors that same year. Today, we refer to RCH in the presence of CNS hemangioblastoma as von Hippel-Lindau disease (VHL).1,2
VHL, one of the phakomatoses, is an autosomal-dominant, multisystem familial cancer syndrome that has been linked to chromosome 3.1,2 Patients who present with isolated retinal capillary hemangiomas should undergo a work-up, including magnetic resonance imaging, to rule out the presence of a CNS tumor.
Our patient has VHL. She reported undergoing removal of a benign brain tumor more than 20 years ago. She also has a strong family history of VHL; her mother and sister have the same condition.
Treatment for the RCH can be difficult and complex. Smaller tumors can be destroyed with photocoagulation and cryotherapy. As tumors enlarge, however, these treatments often are ineffective. The reason: There is so much vascularity and blood within the tumor that treatment often results in hemorrhaging and/or exudative retinal detachment. Laser photocoagulation on the feeder vessel to shut down the blood supply to the tumor has shown some success, although the rapid blood flow through these tumors makes it very difficult to fully choke off the blood supply long enough to allow the tumor to shrink.
The most effective treatments currently include external beam radiation, plaque radiotherapy, gamma knife irradiation and transpupillary thermotherapy (TTT). Anti-VEGF (vascular endothelial growth factor) therapy may also be a viable treatment option, though specific agents are not yet available. Any of these treatments can be done alone or in combination.
Our patient underwent external beam radiation followed by TTT of the two larger tumors and laser photocoagulation of the smaller supertemporal tumor. Unfortunately, she developed a retinal detachment that needed a vitrectomy, scleral buckle and silicone oil. She also developed a cataract that needed removal. Visual acuity eventually stabilized at 20/400.
1. Hinz BJ, Schachat AP. Capillary hemangioma of the retina and von Hippel-Lindau disease. In: Ryan SJ. Schachat AP, Murphy RP (eds). Retina. Volume I: Tumors of the Retina, Choroid and Vitreous. 3rd ed. St. Louis: Mosby, 2000:576-89.
2. Char DH. Retinal tumors. In: Char DH. Tumors of the Eye and Ocular Adnexa (Atlas of Clinical Oncology). American Cancer Society. London: BC Decker Inc, 2001:239-49.
Answers: (1) c; (2) d; (3) a; (4) a; (5) a; (6) c.

