 |
A 65-year-old African American male presented to the primary care clinic complaining of irritation and foreign body sensation in his right eye. He had excessive tearing and couldn’t close his right eye. His symptoms began two weeks prior, following a chemotherapy session.
The patient is currently being treated for multiple myeloma and hypertension. He recovered from hepatitis and prostate cancer 15 years ago, which was treated with radiation. He also reported multiple spinal fractures and open-heart surgery over 20 years ago.
The patient denied diplopia, headache and loss of vision as well as any neurological symptoms of unilateral weakness or slurred speech. His entering blood pressure was high at 160/100mm Hg, but he denied chest pain, headache, shortness of breath and dizziness.
 |
| Fig. 1. The patient suffers from paralysis of the right side of the face in primary gaze. Click image to enlarge. |
Case Findings
The patient’s entering best-corrected visual acuities were 20/30 OD and 20/20 OS. Pupil and motility testing revealed no abnormalities. His confrontation visual fields were unremarkable OU. Slit lamp examination revealed a quiet anterior chamber OU, conjunctival injection with lagophthalmos OD and significant superficial keratitis OD. His intraocular pressures were measured at 15mm Hg OU. Dilated fundus examination revealed arterial attenuation but no other notable pathology. The patient displayed a right-sided facial palsy involving the upper and lower face (Figures 1-3).
Since motility and cover testing did not reveal any significant deviation or underaction, we determined that cranial nerves III, IV and VI were unaffected. The patient’s corneal sensation was intact, as were the maxillary and mandibular branches of the trigeminal nerve. We assessed the patient for balance and gait issues to rule out cranial nerve VIII involvement. He denied any dampening of sound or hyperacusis, which would indicate involvement of the stapedius muscle—a common occurrence in Bell’s palsy. Our assessment of cranial nerves IX through XII was unremarkable as well.
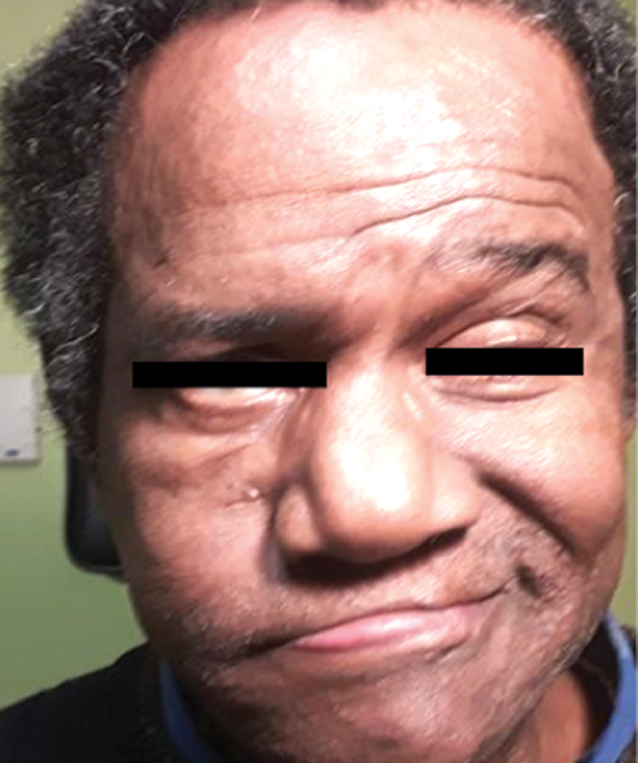 |
Fig. 2. Weakness of the frontalis muscle, orbicularis oculi and lower cheek are notable in stasis and while frowning. Click image to enlarge. |
We performed Humphrey visual field testing to rule out field loss and cerebral involvement (Figure 4). Our results were moderately reliable and did not indicate cerebral involvement or neurological field defect. Assessment of the optic nerve found well-perfused tissue with distinct margins and no evidence of optic atrophy, edema or excavation. OCT showed no significant retinal nerve fiber layer (RNFL) dropout or signs of optic neuropathy OD or OS (Figure 5).
We promptly referred the patient for a gadolinium-enhanced MRI of the parotid gland, temporal bone and brain. The MRI did not reveal metastasis, neoplasm or tissue enhancement. Enhancement of the cranial nerve VI nucleus in Bell’s palsy is reported in 57% to 100% of patients. A lack of enhancement is considered a good prognostic sign.
We ordered serologic testing, including CBC with differential, ESR, Lyme anti-body, Epstein-Barr titer, FTA-ABS, RPR and ANA, in coordination with the patient’s oncology team. There was no indication of an inflammatory or infectious cause of the patient’s condition.
Follow-up
After two weeks of treatment with topical lubricants, the patient returned for a follow-up exam. He reported good ocular comfort with topical lubrication, and his corneal epithelium had significantly improved. His visual acuity had improved to 20/25+1 OD, and we observed a mild improvement in his orbicularis oculi function. The patient could now completely close his right eye with minimal effort (Figure 6).
He came in again after six weeks, during which time his muscle function had continued to improve with no residual weakness or synkinesis.
 |
| Fig. 3. The patient is unable to forcefully close his right eye due to orbicularis weakness. Click image to enlarge. |
Discussion
Bell’s palsy, also known as facial nerve palsy, is a common clinical presentation seen in the primary care setting. It is defined as an acute, ipsilateral facial nerve (cranial nerve VII) paralysis of unknown etiology that results in weakness of the platysma and muscles of facial expression.1,2 Bell’s palsy is the most common disorder that affects the facial nerve and is responsible for about 80% of all facial mononeuropathies.3 Its annual incidence is 15 to 30 per 100,000 people, with equal numbers of men and women affected.2,3
Bell’s palsy is a diagnosis of exclusion; therefore, a thorough medical history and review of systems are paramount in assessing the risk of a systemic cause.1-3 Conditions that may mimic Bell’s palsy include CNS neoplasms, stroke, HIV, multiple sclerosis, Guillain-Barré syndrome, Ramsay Hunt syndrome, Melkersson-Rosenthal syndrome, Lyme disease, otitis media, cholesteatoma, sarcoidosis, trauma to the facial nerve, autoimmune diseases—such as Sjögren’s syndrome—and metabolic disorders, including diabetes.3
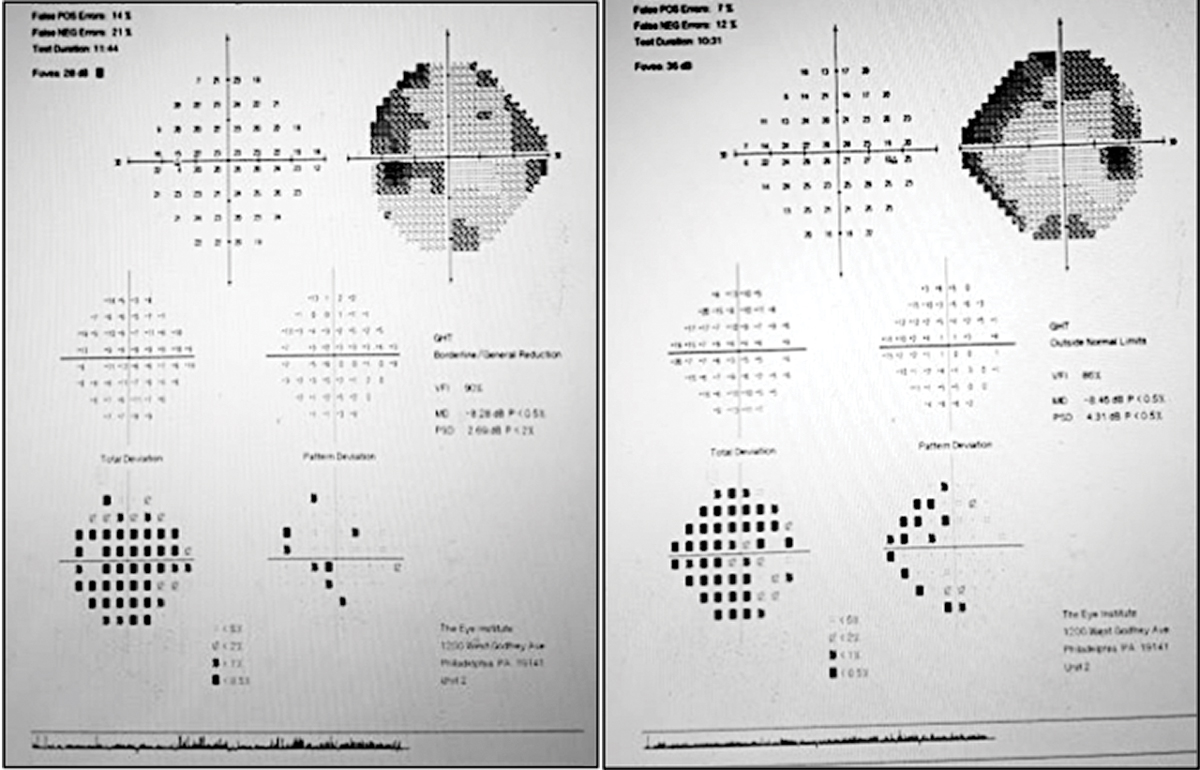 |
Fig. 4. Humphrey visual field testing of the left eye (left) and right eye (right) shows some points of loss inferior to fixation OD and superior nasal OS. Click image to enlarge. |
Idiopathic facial palsy is believed to have an inflammatory pathophysiology. Herpes simplex virus (HSV) activation has been implicated, though the evidence is not entirely conclusive.3,4 HSV-1 genomes were identified in the facial nerve endoneurial fluid and auricular muscles of 11 of 14 patients undergoing decompression surgery for Bell’s palsy but in no controls.3-5
Management is geared toward reducing facial nerve inflammation and preventing corneal complications that stem from paresis of the facial muscles and depends on the underlying etiology. When Bell’s palsy presents acutely, stroke or cerebrovascular incident must be ruled out as the cause of the facial weakness.2,3,5 Signs of a stroke include slurred speech, unilateral weakness, vision loss, dizziness and disorientation. Immediate referral to the emergency room is warranted if any of these signs are noted.
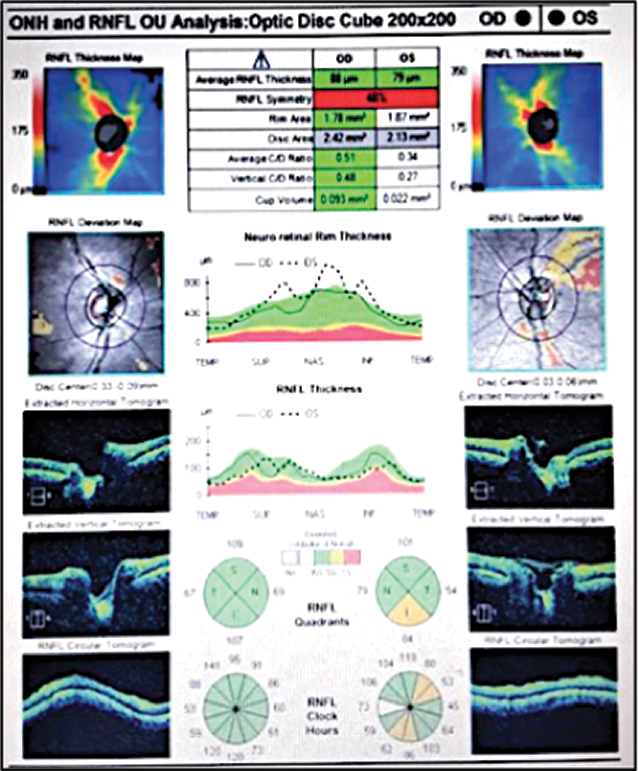 |
| Fig. 5. OCT imaging shows no evidence of RNFL dropout OD and borderline thin RNFL superior temporal to the disc OS. Click image to enlarge. |
Corticosteroids are currently the drug of choice when medical therapy is needed.3,6 Early treatment with oral glucocorticoids within 72 hours of onset has been shown to expedite the resolution of paralysis with limited residual symptoms.6 The suggested regimen is 60mg to 80mg of prednisone per day for one week, after which point it should be tapered off by 10mg per day.3,6,7
Our patient in this case was initially seen after the 72-hour window, so we did not prescribe an oral medication. Oral antivirals have been widely prescribed as monotherapy or in combination with steroids; however, their effectiveness for Bell’s palsy is widely debated.3,4,8
The primary objective in cases of Bell’s palsy is to maintain corneal integrity. Topical lubrication is the first-line treatment and can be prescribed QID or even as often as Q1H depending on the severity of the condition. If corneal integrity is highly compromised, moisture goggles, amniotic membrane therapy or tarsorrhaphy may be indicated. The literature shows no consensus for the benefit of, or indication for, surgery in the treatment of Bell’s palsy.3,6
Patients who do not fully recover their facial function can have varying degrees of facial weakness, hypertonia and synkinesis, which can all be managed with physical therapy.3,4,6 Synkinesis results from post-paralytic re-innervation of different muscles by axons from the same motor neuron. An example found in (aberrant) Bell’s palsy regeneration is eyelid closure when a patient smiles. Botulinum toxin injections may benefit patients with synkinesis, facial spasm or hyperlacrimation.3,6 Weight insertion into the upper eyelid or tarsorrhaphy can improve eyelid closure. Cosmetic and functional improvement may be possible with facial reanimation surgery. Most surgeons will not perform reanimation surgery unless no improvement has been noted for at least nine months.
 |
Fig. 6. The patient’s orbicularis function visibly improved by his six-week follow-up. Click image to enlarge. |
Patients with Bell’s palsy will have a favorable prognosis if some recovery is seen within the first 21 days of onset and should have some notable recovery by four months after the onset of symptoms.3,6 If no improvement is noted by then, repeat imaging and additional work-ups may be indicated. An MRI delineates the soft tissue structures and is the best way to evaluate the intraparotid facial nerve for inflammation, edema or neoplasm.
When a patient presents with acute onset facial nerve palsy, a thorough history and physical examination should be performed. The clinician must selectively test the involved muscles of the face and order additional neurological and serological testing as necessary to further assess for pathology.
Although our suspicion for Bell’s palsy was high at the onset, this patient had several underlying conditions, including metastasis, stroke and infection, that complicated the case. This highlights the importance of fully evaluating a high-risk patient who presents with neurological abnormalities in a primary care setting.
Dr. Gretz provides comprehensive eye care with a focus on ocular disease and emergency medicine at Simon Eye Associates and is a member of the Delaware Optometric Association and the American Optometric Association. He graduated from the Pennsylvania College of Optometry at Salus University in 2018, where he completed a residency in primary care and ocular disease.
1. Tiemstra JD, Khatkhate N. Bell’s palsy: diagnosis and management. Am Fam Physician. 2007;76(7):997-1002. 2. May M, Klein SR. Differential diagnosis of facial nerve palsy. Otolaryngol Clin North Am. 1991;24(3):613-45. 3. Zandian A, Osiro S, Hudson R, et al. The neurologist’s dilemma: a comprehensive clinical review of Bell’s palsy, with emphasis on current management trends. Med Sci Monit. 2014;20:83-90. 4. Baringer JR. Herpes simplex virus and Bell palsy. Ann Intern Med. 1996;124(1 Pt 1):63-5. 5. May M, Galetta S. The facial nerve and related disorders of the face. In: Glaser JS (ed.), Neurophthalmology (2nd ed.), Philadelphia, J. B. Lippincott Co., 1990:239-77. 6. Baugh RF, Basura GJ, Ishii LE, et al. Clinical practice guideline: Bell’s palsy. Otolaryngol Head Neck Surg. 2013;149(3 Suppl):S1-27. 7. Salinas RA, Alvarez G, Ferreira J. Corticosteroids for Bell’s palsy (idiopathic facial paralysis). Cochrane Database Syst Rev. 2004;(4):CD001942. 8. Hato N, Sawai N, Teraoka M, et al. Valacyclovir for the treatment of Bell’s palsy. Expert Opin Pharmacother. 2008;9(14):2531-6. |

