Annual Dry Eye ReportCheck out the other feature articles in this month's report: |
Ocular surface disease can complicate and, in some cases, impede cataract surgery. At least one study shows 63% of presurgical cataract patients have a decreased tear break-up time (TBUT) of five seconds or less—indicating evaporative dry eye.1 That same research shows 77% of patients scheduled for surgery had corneal staining.1 Other research indicates that 87% of cataract patients use artificial tears one month postoperatively.2
While dry eye is now a widely diagnosed disease, the number of actual sufferers is likely even greater since many self treat using over-the-counter products or underreport their symptoms. I’ve heard patients say they believe ocular dryness is simply “typical for my age.” However, dry eye disease (DED) can have significant consequences to a patient’s lifestyle as well as on various aspects of cataract surgery. As primary care clinicians, optometrists need to take special consideration of the ocular surface health of every patient planning to undergo cataract surgery. This includes gathering preoperative measurements, and monitoring postoperative refractive outcomes.
Here, we review how to oversee the health and stability of a cataract patient’s ocular surface, before and after the operation. We will also explain how stabilizing the ocular surface before surgery can impact post-op satisfaction and reduce the chances of possible complications.
 |
| Eyelid warming devices such as the Tearcare system (Sightscience), can help express meibmoian glands and prepare the patient for refractive surgery. Click image to enlarge. |
Test All, Despite Symptoms
Patients who are symptomatic will likely be more receptive to discussing how their DED can affect surgery. Generally speaking, these patients may or may not want to have the dry eye treated prior to surgery but patients may not fully understand the impact that a compromised ocular surface can have on their surgical outcomes.
Research clearly shows an impaired ocular surface affects preoperative planning for cataract surgery.3 Having a poor tear film can potentially alter the corneal surface resulting in reduced repeatability of keratometry readings and diminished accuracy of intraocular lens (IOL) calculations.3 The study also concluded that diagnosing and treating dry eye preoperatively results in better visual outcomes.3 However, many patients present asymptomatically. Only approximately 22% of the patients presenting for surgery had been diagnosed with dry eye previously.1 However, a 2015 study shows dry eye in 54.3% of 400 participants older than 40 years.4 Additionally, that study shows the prevalence is greatest among participants 71 years or older (67.3%), around the age when many will also be facing potential cataract surgery.4,5 Of those who reported being completely asymptomatic, 24.1% had dry eye.4
Patients with subclinical DED are just as likely to experience surgical complications and return with one or more DED symptoms. So, the importance of dry eye testing using both signs and symptoms for every cataract surgery candidate can’t be overstated.
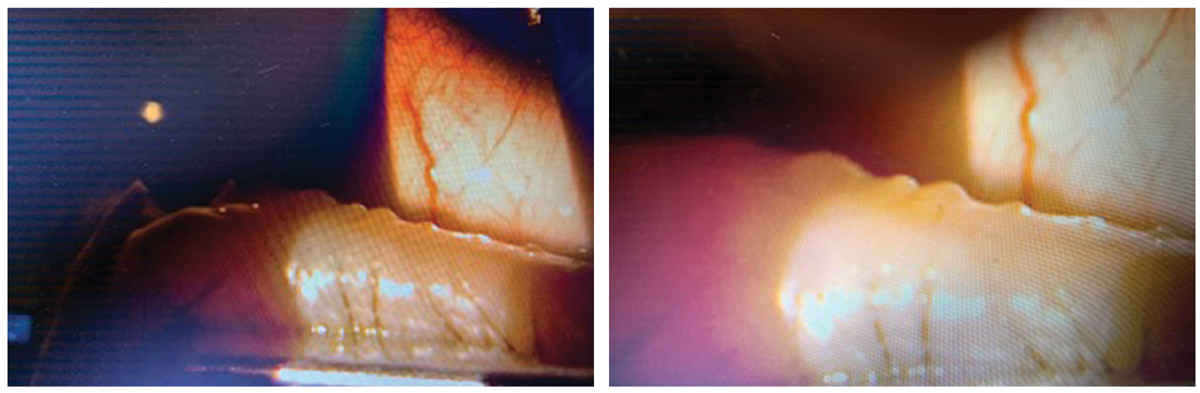 |
These slit lamp images show a patient undergoing the TearCare procedure. Note the visible material being expressed from the glands. Click image to enlarge. |
Create a Testing Protocol
Any discussion about how to treat ocular surgery patients with dry eyes needs to begin with identifying the problem. In our clinic, we stick close to the American Society of Cataract and Refractive Surgery (ASCRS) guidelines.6 By measuring patient symptoms via SPEED questionnaires, we are able to determine the patient’s perspective of their condition preoperatively. We repeat the questionnaire at each visit (except day one and week one post-op). In our clinic, we flag scores higher than 8 as dry eye suspicious. This step is important because, as we’ve likely all heard before, “If a patient is diagnosed prior to surgery, it is the patient’s problem, if a patient is diagnosed after surgery, it is the doctor’s problem.”
Other measures of subjective symptoms include the Dry Eye Questionnaire-5 or the Ocular Surface Disease Index. Whichever test you employ, this subjective information is especially valuable when combined with the same results after the procedure. Often, patients present postoperatively with what they perceive is DED caused by their cataract surgery. By referencing a pre-op questionnaire, it frequently reveals that the same symptoms were present before the procedure as well. It can reassure a patient to learn that the surgery did not worsen their dry eye, only that they are now more aware of the symptoms.
Objective tests are also critical in identifying patients, especially those who are asymptomatic. But even if patients are symptomatic, objective DED tests can reveal much about the current homeostasis of the patient’s tear film, so you’ll want to incorporate some of the following into your preoperative workup. In our clinic, we have access to both inflammatory marker measurements (Inflammadry, Quidel) and tear osmolarity measurements (Tearlab). When combined with TBUT, osmolarity measurements provide an adequate assessment based on the Tear Film and Ocular Surface Society’s DEWS II definition.7
Tear hyperosmolarity correlates strongly to tear film instability. A 2017 study shows patients with hyperosmolarity had a greater corneal variability as measured with keratometry readings, resulting in IOL calculation variability as well.8 With the addition of this purely objective data, a provider can effectively identify a significant number of dry eye patients preoperatively. Other investigative options can include tear film interferometry, tear clearance assessments (i.e., fluorescein clearance test, tear function index, fluorophotometry) and ocular surface damage assessment (i.e., corneal and conjunctival, rose bengal, lissamine green staining, cytology), corneal epithelial cell mapping and lipid layer assessments (i.e., precorneal/meibomian grading).9
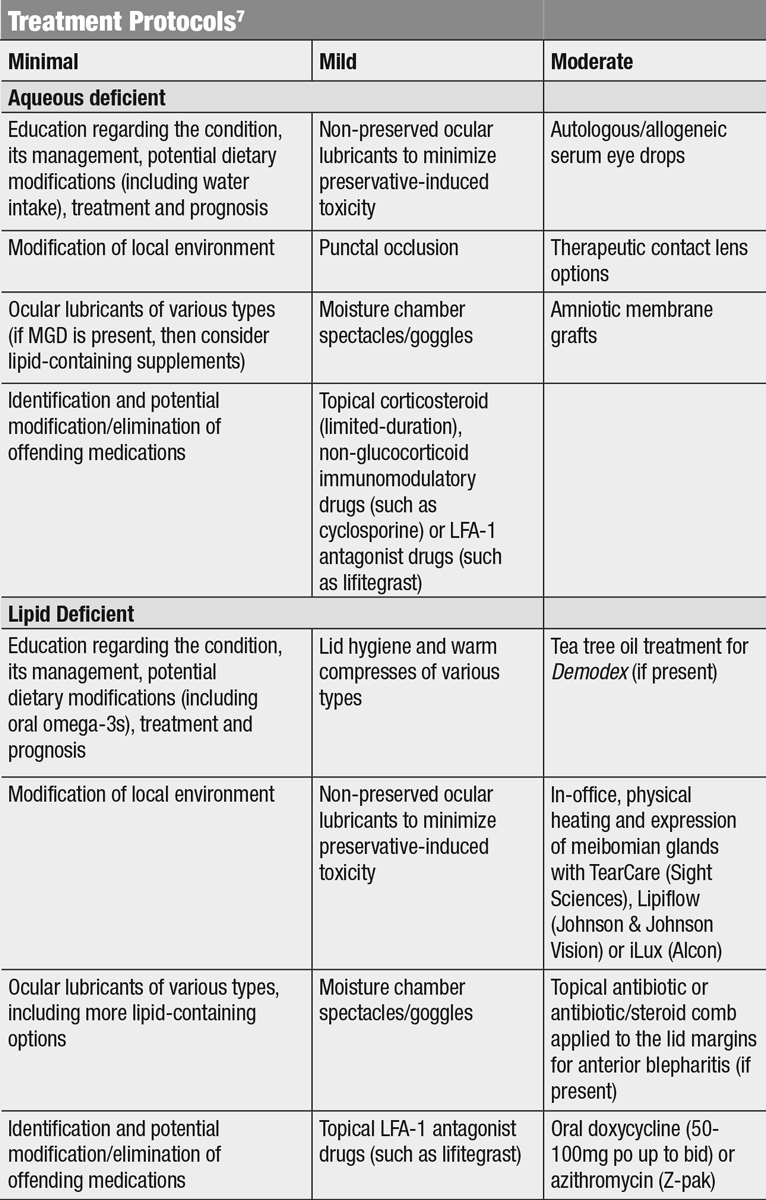 |
| Click table to enlarge. |
Presurgical Treatment
With appropriate identification, optometrists can customize the most appropriate treatment plan for each patient. This can help determine the best procedure as well as the most appropriate IOL for the patient. A patient with significant history of DED may not be the best candidate for a multifocal lens since these lenses typically require high contrast to maximize the vision. DED identification in premium IOL patients is not only critical for the success of the patient but also for the success of the refractive cataract surgery portion of the practice since many of these patients are paying out of pocket and bring higher expectations of their surgical results. In attempting to meet the higher expectations of refractive cataract lens patients, providers should have a healthy ocular surface prior to surgery as a priority in their treatment plans.
Surgical delay. One way to establish a healthy ocular surface is by stabilizing the ocular tear film while delaying the surgery. Reasons to delay surgery include corneal abnormality (e.g., dellen, superficial punctate keratitis), irregularity in kerotometry (topography) measurements or fluctuating vision.
If delaying the procedure is warranted, it is important to understand what is being monitored so treatment can be appropriate and an endpoint can be achieved. This process can take two to four weeks or longer to improve adequately enough to proceed with surgery. Only upon adequate resolution of the signs and symptoms should the patient proceed. For most patients planning to have standard IOLs implanted, we’ve found that a 70% resolution of staining is fine as long as the central area is cleared. The same would apply to symptoms—if a patient’s symptoms are reduced by 25%, they may be improved enough to proceed, although this is not a hard and fast rule as some contingencies can impact the decision.
Ocular surface issues have an outsized effect on the performance of multifocal IOLs, so if your patient is interested in these high-performance lenses, it is imperative that they achieve a healthy tear film prior to surgery. For example, if a patient with SPK chooses a traditional IOL, they may be counseled as to the effects of the SPK on their vision and it may be treated concomitantly. If the same patient desires a multifocal IOL, however, their dry eye will more profoundly affect their postoperative vision and should be resolved prior to surgery. Apply the same rationale to epithelial thickness and keratometry
measurements with an emphasis on stability. Take these measurements on a serial basis to determine whether or not the surface is stable. TBUT can create irregular dynamic acuity and becomes a much greater concern with multifocal IOLs, where the patients report transient decreases in vision that are attributable to variations in tear film causing decreased contrast sensitivity.10
 |
| This meibography picture demonstrates mild breakdown of the meibomian glands. Classic signs in this image are the lack of parallel meibomian gland structures—whether due to angling or breakdown. Click image to enlarge. |
Treatment. As their are different possibilities to treat the ocular surface, much depends on the etiology. If patients lack sufficient tear volume—based on tear meniscus height in conjunction with qualitative analysis of the lipid layer—prescribing a cyclosporine option may be the best option, or punctal occlusion if no inflammation present. However, if the source is MGD, thermal treatments with expression may be the best option. Doxycycline can also be considered in patients with MGD. If the patient shows significant SPK, loteprednol or lifitegrast may be prescribed or in severe cases an amniotic membrane can be employed. In the least, good hygiene and some form of preservative free artificial tears and/or warm compresses can likely be of help to these patients whether it is used prior to surgery, during the postoperative period (excluding warm compresses during the first week), or for long term maintenance.
When performing the biomicroscopy exam, pay special attention to corneal and conjunctival structures to note any staining. Don’t forget to also evaluate the patient’s tear meniscus. Additionally, note the lid margin health to determine the state of the glands and the status or potential status of any lid infections or inflammations that could potentially disrupt postoperative healing. Meibomian gland expression can be performed using the Meibomian Gland Evaluator (Johnson & Johnson Vision) to demonstrate gland function. During the clinical exam the provider should also pay special attention to mechanical or structural abnormalities such as poor lid closure, inadequate lid apposition or an irregular lid margin.
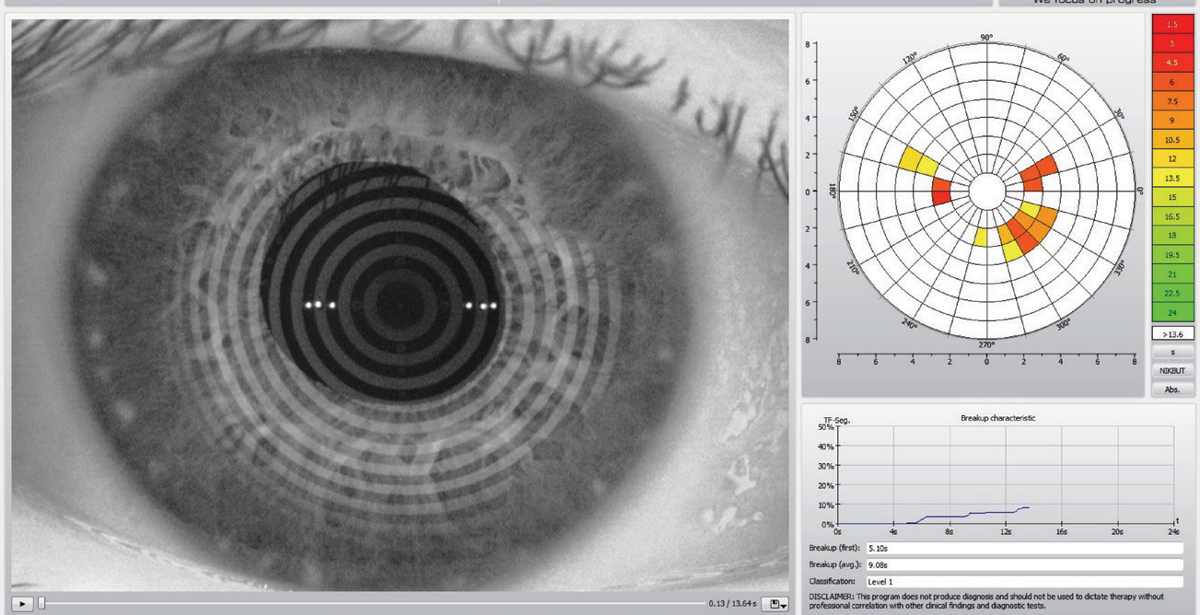 |
| This Keratograph 5M (Oculus) images is can help establish a patient’s tear break-up time, which can help prepare them for surgery. Photo by Dan Fuller, OD. Click image to enlarge. |
Anterior Healing
During the immediate postoperative period, several complications may arise. These include acute intraocular pressure spikes, endophthalmitis and cystoid macular edema. These can occur with any patient—dry eye or otherwise—following traditional cataract surgery, laser-assisted cataract surgery or refractive cataract surgery. However, for a patient who was previously diagnosed and treated for DED prior to surgery, the optometrist needs to educate them about their normal healing course. You’ll need to explain that the use of topical antibiotics and antinflammatories and the preservatives located within them can potentially lead to ocular surface agitation, leaving patients with a newly observed or heightened awareness of DED symptoms.11
Counsel patients who traditionally use warm compresses to manage posterior blepharitis or use lid scrubs to manage anterior blepharitis to withhold these therapies for a full week, so as not to compromise the new incision and create any increased risk for infection. Stopping these maintenance regimens can lead to a potential backslide or relapse of previously managed DED.11
Exposure to light from the operating microscope can also be a contributing factor to the patients dry eye syndrome.12-14 Optometrists should explain to patients that even the corneal incision can potentially exacerbate a patient’s DED. The incision itself can potentially cut through the nerves that are responsible for innervating the corneal surface and, by doing so, may delay the epithelial wound healing. Discussing this helps the patient understand that, during the initial healing process, they may have reduced tear production, decreased TBUT, decreased mucin production increased inflammation and, ultimately, discomfort.15 This aspect is relatively temporary and will correct itself with healing.
 |
The iLux (Alcon) can be performed in the office to help clear the meibomian glands of patients with dry eye due to meibomian gland dysfunction. This can help set the stage for a successful refractive surgery. Click image to enlarge. |
Outcomes
It is not uncommon for a patient to have an outstanding surgical procedure, yet be unsatisfied with the outcome.10 In a 2016 study of patients who were dissatisfied, 57% were due to refractive error and 35% were due to DED. Patients may also confront postoperative discomfort as a result of the previously mentioned postoperative drops, but some might develop discomfort due to a preoperative refractive miscalculation as any residual refractive error can produces eyestrain or create anisometropia between the two eyes. These patients can have uncorrected 20/20 vision, yet exhibit “20/unhappy” presentation. Since refractive error is closely associated with dry eye, it’s worthwhile to evaluate the ocular surface.16
It is imperative to reset expectations during this timeframe. Missed refractive errors can be modified, but it is important to correct the underlying condition that may have caused the error. Likewise, if the post-operative course is expected to be temporary, take measures to address the problem and counsel the patient.
Since dry eye disease can have an influence on ocular surgery before and after the procedure, providers should recognize the condition and treat it appropriately. For some, that treatment means delaying the procedure so the condition can be minimized or corrected, while for others it may just mean a more thorough education on appropriate expectations. However, all eye care providers should be aware of the impact this condition can have as well as the resulting consequences if they are not dealt with appropriately.
Dr. Chester is a partner at the Cleveland Eye Clinic and is active in training professionals in the perioperative care of the refractive surgery patient, cataract surgery co-management and ocular surface disease management.
1. Trattler W, Majmudar P, Donnenfeld E, et al. The prospective health assessment of cataract patient (PHACO) study: the effect of dry eye. Clin Ophthalmol. 2017;11:1423-30. 2. Roberts CW, Elie ER. Dry eye symptoms following cataract surgery. Insight 2007;32(1):14-21. 3. Chuang J, Shih KC, Chan T, Wan KH, Jhanji V, Tong L. Preoperative optimization of ocular surface disease before cataract surgery. J Cataract Refract Surg. 2017;43(12):1596-1607. 4. Shah S, Jani H. Prevalence and associated factors of dry eye: our experience in patients above 40 years of age at a tertiary care center. Oman J Ophthalmol. 2015;8(3):151–6. 5. Kauh C, Blachley T, Lichter P, et al. Geographic variation in the rate and timing of cataract surgery among US communities. JAMA Ophthalmol. 2016;134(3):267-76. 6. Starr C, Gupta P, Farid M, et al. An algorithm for the preoperative diagnosis and treatment of ocular surface disorders. J Cataract Refract Surg. 2019;45(5):669-84. 7. Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15(3):276-83. 8. Epitropoulos AT, Matossian C, Berdy GJ, et al. Effect of tear osmolarity on repeatability of ketratometry for cataract surgery planning. J Cataract Refract Surg. 2018; 44(9):1090-6. 9. Kanellopoulos A, Asimellis G. In pursuit of objective dry eye screening clinical techniques. Eye Vis (Lond). 2016;3:1 10. Gibbons A, Ali T, Waren D, Donaldson K. Causes and correction of dissatisfaction after implantation of presbyopia-correcting intraocular lenses. Clin Ophthalmol. 2016;10:1965–70. 11. Walsh K, Jones L. The use of preservatives in dry eye drops. Clin Ophthalmol. 2019;13:1409-25. 12. Sutu C, Fukuoka H, Afshari N. Mechanisms and management of dry eye in cataract surgery patients. Curr Opin Ophthalmol. 2016;27:24-30. 13. Cho Y, Kim M. Dry eye after cataract surgery and associated intraoperative risk factors. Korean J Ophthalmol. 2009;23:65-73. 14. Li X, Hu L, Hu J, Wang W. Investigation of dry eye disease and analysis of the pathogenic factors in patients after cataract surgery. Cornea. 2007;26(9 Suppl 1):S16–S20. 15. Donnenfeld ED, Solomon K, Perry HD. The effect of hinge position on corneal sensation and dry eye after LASIK. Ophthalmology. 2003 May; 110(5):1023-30. 16. Dhungel D, Shrestha G. Visual symptoms associated with refractive errors among Thangka artists of Kathmandu valley. BMC Ophthalmol. 2017;15:258. |

