Recurrent corneal erosion (RCE) is a clinical syndrome characterized by inadequate epithelial basement membrane adhesions, resulting in repeat episodes of corneal epithelial defects.1 These episodes are typically acute and may involve symptoms ranging from mild irritation to significant pain.1-3 The average age of onset is the fourth or fifth decade, with a slight female predominance.1,3
It’s a condition that can leave patients with a fair amount of discomfort. Luckily, the optometrist can help. This article offers keys to understanding RCE, its diagnosis and treatment options.
Diagnosis
RCE is diagnosed based on clinical signs and patient history, so a thorough history is necessary; don’t forget to ask about prior episodes of corneal trauma.1 Patients will typically describe symptoms that occur during sleep or upon awakening and may include redness, photophobia and tearing.1,2
While the lids are closed during sleep, superficial epithelial edema may lead to decreased epithelial adhesion. Opening of the lid or rapid eye movement produces a shearing force on the epithelium, leading to erosion.3 Corneal signs may range from focal superficial punctate keratitis to a full-thickness epithelial defect.1
A detailed slit lamp examination should be performed with fluorescein staining and retroillumination, and the fellow eye should be examined for signs of basement membrane dystrophy.1
Microform erosions consist of minor episodes lasting as little as 30 minutes and typically have an intact corneal epithelium upon examination.2,4 Macroform erosions are more severe episodes with epithelial defects or areas of edematous, poorly adherent epithelium. These may last for days and are associated with severe pain, eyelid edema, decreased visual acuity and extreme photophobia.2,4
If an exam does not reveal obvious epithelial defects, an adhesion test can assess for inadequate epithelial-stromal adhesion. A dry cellulose surgical sponge is gently passed over the area of suspected epithelium. If the intact epithelium is movable, the adhesion test is positive.1
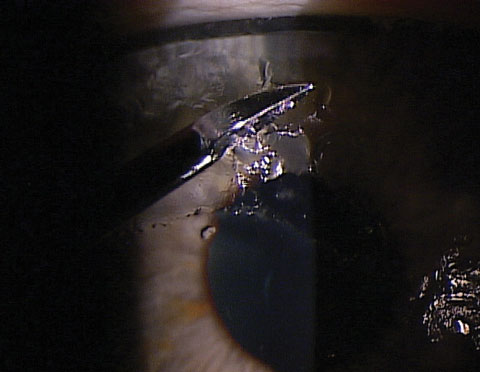 |
| Optometrists can debride the epithelium at the slit lamp under topical anesthesia using a foreign body spud. |
Etiology and Pathophysiology
RCE is commonly associated with prior corneal trauma or underlying corneal disease. The most common underlying etiologies are trauma (45% to 69%) and epithelial basement membrane dystrophy (EBMD) (20% to 30%).1 Causative trauma is typically a shallow corneal injury such as an abrasion from a fingernail, piece of paper, or tree branch.3 Prior trauma classically leads to macroform erosions.3 In contrast, EBMD classically leads to microform erosions.3 The estimated incidence of RCE following traumatic corneal abrasion ranges from 5% to 25%.1
Normally, the corneal epithelium is anchored to the basement membrane and Bowman’s layer by specialized adhesion complexes. These complexes consist of hemidesmosomes and anchoring fibrils.1 Trauma and corneal dystrophies have the potential to disrupt the adhesion complexes, which predisposes the epithelium to repetitive erosions.1 The exact mechanism of the failure of adhesion complexes is not fully understood, but researchers propose there are pathologies or absence of the basement membrane or hemidesmosomes.3 This leads to repetitive elevation of the epithelium, which causes formation of further abnormalities in the basement membrane.3
Patients with RCE have increased activity of matrix metalloproteinases (MMP)-2 and -9. These enzymes can adversely affect the basement membrane and anchoring fibrils, thereby causing dysfunctional adhesion complexes.1,3 Further, there are high rates of meibomian gland dysfunction (MGD) and ocular rosacea in eyes with non-traumatic corneal erosion.3 Diseases with high colonization of Staphylococcus epidermidis tend to have higher levels of bacterial lipases, which act upon meibum to produce toxic free fatty acids. Investigators believe these fatty acids interfere with the epithelial healing process and predispose patients to erosions.3 Therefore, many medical treatments are aimed at decreasing MMP activity, or managing MGD, or both.
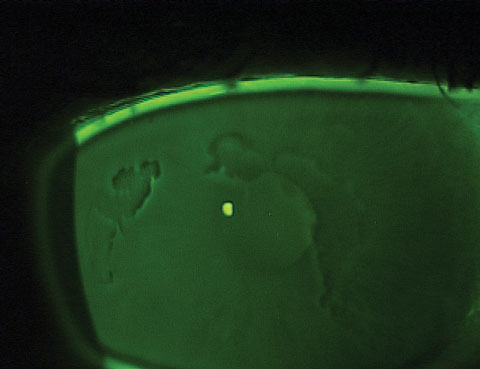 |
| This patient exhibits negative staining at the slit lamp, which is indicative of epithelial basement membrane dystrophy. |
Treatments
The two primary therapeutic goals for RCE are to facilitate rapid re-epithelialization and relieve pain. A secondary goal is to prevent future occurrences of erosion.3 Medical therapy typically results in resolution of the epithelial defect.1 Frequent nonpreserved artificial tears help re-epithelialization, but do not seem to help in the prevention of recurrence.1,3,5
A topical nonsteroidal anti-inflammatory drug (NSAID) may be prescribed to reduce pain, although long-term use should be avoided as they may delay epithelial healing.6 Topical prophylactic antibiotics should be used to decrease the risk of microbial keratitis.1 For large epithelial defects or patients in significant pain, oral opioids (such as hydrocodone with or without acetaminophen) may be necessary to provide adequate pain control.7
Medical therapy is typically the initial therapeutic choice to prevent recurrences, although 60% will have persistent symptoms following medical treatment.8 Treating underlying lid disease, such as MGD and blepharitis, significantly decreases the frequency of recurrent erosions.9 MMP-9 inhibitors, such as topical steroids and doxycycline, also speed resolution and help to prevent further recurrences.10 Topical ointments may be used at bedtime for lubrication. These are often continued for several weeks until the epithelium is tightly adhered to the stroma.1 Hypertonic ointments are often prescribed at bedtime for weeks to months to complete deturgescence of the corneal epithelium and improve adhesion.11 However, these ointments may be irritating for some patients due to the salt content.1 Hypertonic drops may also be helpful (and less irritating), although the contact time of a drop is less than an ointment. Erythromycin ointment provides some antibiotic prophylaxis and may reduce MMP-9.1,11 The use of autologous serum may be effective at preventing recurrence in select patients.3
Bandage contact lenses are often used to protect the epithelium from the shearing force of the lids.1,12 When using a bandage lens, the clinician should take care to avoid tight lens syndrome.1 This condition involves acute tightening of the contact lens, which leads to decreased lens movement, inflammatory debris beneath the lens, increased inflammation and pain.1 The use of a relatively flat base curve and topical NSAIDs can help avoid tight lens syndrome.1 Nonpreserved artificial tears help to flush inflammatory debris and improve comfort. Topical prophylactic antibiotics should be used to decrease the risk of microbial keratitis, which may be caused by extended use of bandage soft lenses.1,11 Patients may wear bandage contact lenses continuously for six to 12 weeks to allow for restoration of tight epithelial basement membrane adhesions.13 The lens must be replaced as appropriate.1,2
Despite treatment of acute episodes, some patients will continue to have minor and major RCE occurrences. For recalcitrant cases, surgical therapy may be necessary. Surgical intervention helps to prevent further recurrences by stimulating new and stronger epithelial adhesion complexes.1,2,8
Epithelial Debridement
Mechanical debridement of loosely adhered or nonadherent epithelium provides a smooth basement membrane to which healthy epithelium may re-adhere.1 This is a safe and relatively noninvasive procedure that is typically performed at the slit lamp under topical anesthesia.1,8 The patient is prepared by instilling topical anesthetic in both eyes.2 Topical prophylactic antibiotics may be used, and an eyelid speculum is often helpful.2 Depending upon practitioner preference, various instruments may be used to remove loose epithelium.8 A methylcellulose spear-shaped surgical sponge (i.e., Weck-cel) is a safe and effective option.1,8,14 A Kimura spatula may also be used since its blunt edges make it unlikely to damage Bowman’s membrane.2,8 Occasionally, sharper instruments such as a scalpel blade are sometimes advocated; other authors contend that sharp instruments are inappropriate for this.1,2 Remove any loose epithelial debris with jeweler’s forceps or a cellulose surgical sponge.8
Loose epithelium is removed to the point of tight adherence.11 Aggressive removal of the epithelium near the limbus can damage stem cells; therefore, a protective band of epithelium should be maintained 1mm to 2mm from the limbus.3,8 Bowman’s layer is lightly debrided to remove the epithelial basement membrane.2 Cyclopentolate is instilled.11
A bandage contact lens should be placed for two days to two weeks, and topical antibiotics and nonsteroidal drops prescribed.2 Bedtime ointment may be considered for three to six months.2
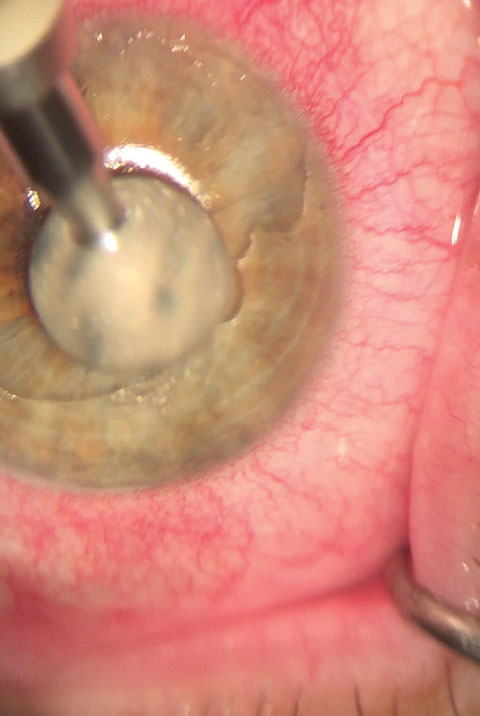 |
| A diamond burr can be used to lightly buff Bowman’s layer until a smooth surface is achieved. Photo: Nathan Lighthizer, OD |
Diamond Burr Polishing
Following debridement of loose epithelium, diamond burr polishing may be performed. Compared with simple debridement, polishing may remove more abnormal basement membrane. This can provide a smoother surface and stronger epithelial-stromal adhesion, which should enhance the outcome.14
Diamond burr polishing may be safely performed at the slit lamp with a handheld, battery operated 5mm diamond burr.11,14 After debriding loose epithelium as described previously, a diamond burr is used to lightly buff Bowman’s layer until a smooth surface is achieved.2,14 This takes approximately five to 10 seconds, although some sources advocate up to 30 seconds.8,14 Vertical or circular motions may be employed.8,14 Vigorous polishing should be avoided, as it may breach Bowman’s layer and cause postoperative corneal haze.14
A bandage contact lens is placed, and antibiotic and nonsteroidal drops are prescribed.2
Anterior Stromal Puncture
This technique, which has been compared to spot welding in metalworking, is performed at the slit lamp under topical anesthetic. Multiple shallow penetrations are made through the epithelium into the anterior stroma. This forms scarring attachments and improves epithelial adhesion.15 Specialized instruments may be used to prevent corneal perforation. Stromal puncture may be performed through loose epithelium without performing debridement. Fluorescein helps to visualize puncture marks. Topical NSAIDs should be used to control postoperative pain. Prophylactic antibiotics should also be applied to prevent microbial keratitis.15
Punctures should be placed 0.5mm to 1mm apart within the entire erosive area. The treatment zone should extend 1mm to 2mm into normal margins to prevent recurrence. Treatment of the visual axis is controversial; investigators have yet to reach a consensus as to whether stromal puncture causes decreased acuity or glare.15
Transplantation
Amniotic membranes exert anti-inflammatory and anti-scarring effects on tissue.16 They contain tissue inhibitors of MMP-9.16 Transplantation of an amniotic membrane as a biologic bandage may be beneficial following epithelial debridement.16 Techniques for placement of amniotic membrane vary based on the type of membrane used. Antibiotic drops may be used with the membrane in place.16
Expected Outcomes
Debrided epithelium is typically re-epithelialized by three or four days, although this depends on the area debrided.14 There may be mild corneal haze for three to four weeks; this rarely may persist as a long-term complication.8,14
The literature still lacks strong evidence regarding the efficacy of various RCE therapies. A Cochrane systematic review included seven randomized controlled trials, all of which were considered “poor quality.”12 The level of evidence was found to be insufficient for the development of management guidelines.
A double-masked randomized controlled trial in Hong Kong (n=48) compared simple epithelial debridement with debridement with diamond burr polishing.14 The authors found fewer recurrences and less need for repeat intervention in the diamond burr group over six months of follow-up. The incidence of major recurrences was 4% in the diamond burr group vs. 56% in the simple debridement group. Minor symptoms recurred in 20% (diamond burr) vs. 65% (debridement). Additional interventions were needed in none of the diamond burr subjects and 52% of the debridement group.14
Although debridement aids the resolution of the acute erosive episode, evidence that debridement alone can prevent additional episodes is lacking.1,8 However, simple debridement can successfully convert most patients with macroform erosions to microform erosions.2
A small study of 11 eyes with history of RCE examined the effect of amniotic membrane transplantation over 10 to 16 months of follow-up. Eight eyes had previous failure with conservative medical treatments. The authors performed debridement using a surgical sponge followed by placement of amniotic membrane. Only one eye recurred. Interestingly, 10 eyes had improvement in best-corrected visual acuity.16
Recurrent corneal erosion is relatively common, and may not be adequately managed with medications. Surgical intervention may enhance outcomes and reduce recurrences. Epithelial debridement with diamond burr polishing is a safe, effective procedure for the treatment of this condition.
Dr. McNulty practices at Louisville Eye Center in Louisville, Ky. He is vice president of the Kentucky Optometric Association and was named the 2014 Kentucky Young Optometrist of the Year.
|
1. Albert D, Miller J, Azar D. Recurrent corneal epithelial erosion. Albert & Jakobiec’s Principles and Practice of Ophthalmology. Philadelphia: Saunders/Elsevier;2008. 2. Reidy J, Paulus M, Gona S. Recurrent erosions of the cornea. Cornea. 2000;19(6): 767-71. 3. Xu K, Kam K, Young A, Jhanji V. Recurrent corneal erosion syndrome. Asia-Pacific Journal of Ophthalmology. 2012;1(6):349-54. 4. Chandler P. Recurrent erosions of the cornea. Am J Ophthalmol. 1945;28:355-63. 5. Eke T, Morrison DA, Austin DJ. Recurrent symptoms following traumatic corneal abrasion: prevalence, severity, and the effect of a simple regimen of prophylaxis. Eye (Lond). 1999;13(Pt 3a):345Y347. 6. Hersh PS, Rice BA, Baer JC, et al. Topical nonsteroidal agents and corneal wound healing. Arch Ophthalmol. 1990;108:577Y583. 7. Jacobs D. Corneal abrasions and corneal foreign bodies: Management. In: UpToDate, Trobe J. Waltham, MA. Accessed December 16, 2016. 8. Mcgrath L, Lee G. Techniques, indications and complications of corneal debridement. Sur Ophthalmol. 2014;59(1):47-63. 9. Hope-Ross MW, Chell PB, Kervick GN, et al. Recurrent corneal erosion: clinical features. Eye (Lond). 1994;8(Pt 4):373Y377. 10. Dursun D, Kim MC, Solomon A, et al. Treatment of recalcitrant recurrent corneal erosions with inhibitors of matrix metalloproteinase-9, doxycycline and corticosteroids. Am J Ophthalmol. 2001;132:8Y13. 11. Laibson P. Recurrent corneal erosions and epithelial basement membrane dystrophy. Eye & Contact Lens: Science & Clinical Practice. 2010;36(5):315-7. 12. Watson S, Lee M, Barker N. Interventions for recurrent corneal erosions. Cochrane Database of Systematic Reviews. 2012. 13. Fraunfelder F, Cabezas M. Treatment of recurrent corneal erosion by extended-wear bandage contact lens. Cornea. 2011; 30(2):164-6. 14. Wong V, Chi S, Lam D. Diamond burr polishing for recurrent corneal erosions: results from a prospective randomized controlled trial. Cornea. 2009;28:152-6. 15. Brightbill F, Lhowe L, McDonnell P, et al. Corneal surgery theory, technique and tissue 4th ed. Philadelphia, PA, United States: Elsevier Health Sciences;2014. 16. Huang Y, Sheha H, Tseng S. Self-retained amniotic membrane for recurrent corneal erosion. J Clin Exp Ophthalmol. 2013;4:272. |

