History
A 30-year-old white female presented for a routine eye examination. Her ocular history was remarkable for what she called lazy eye.
Her systemic history was noncontributory.
Diagnostic Data
Her best-corrected visual acuity was 20/30 O.D. and 20/20 O.S. at distance and near. External examination was normal, with no afferent pupillary defect. Refraction uncovered mild myopia in both eyes. Anterior segment findings were unremarkable.
Goldmann applanation intraocular pressures measured 14mm Hg O.U. The photographs illustrate the pertinent optic nerve finding. Peripheral dilated funduscopy was within normal limits in both eyes.
How would you approach this case? Does this patient require additional tests? What is your diagnosis? How would you manage this patient? What is the likely prognosis?
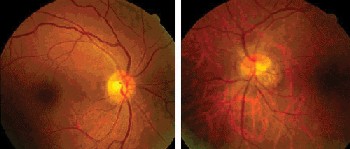 |
| A 30-year-old white female presented with the ocular nerve appearance shown here. |
Discussion
Additional tests included:
Expanded history to rule out strabismus.
Cover testing to rule out strabismus.
Random dot and contour stereo testing to rule out monofixation syndrome.
Worths 4-dot test to rule out suppression.
Reevaluation of the pupillary responses with a neutral density lens filter to rule out optic neuropathy.
Detailed refraction (wet and dry) with keratometry to rule out refractive error or keratoconus.
Amsler grid to rule out gross maculopathy.
Laser interferometry to assess the potential for best-corrected acuity.
The diagnosis in this case is tilted disc syndrome. (Fuchs coloboma is another name that has been applied to the entity.) In an ophthalmoscopy, tilted optic discs often appear to be longer horizontally than vertically. They are usually accompanied by an inferonasal crescent. The tilted disc may be associated with an outpouching of the globe (staphyloma) in the quadrant where the crescent is located (referred to as nasal fundus ectasia).1
Visual acuity in eyes with tilted discs may be normal but often is mildly decreased. In those with fundus ectasia, a relative temporal field defect may be uncovered. In bilateral cases, these abnormalities have the potential to produce bitemporal hemianopia.
The treatment is patient education and full-time polycarbonate protection.
1. Alexander LT. Congenital and acquired anomalies of the optic nerve head. In: Alexander LS. Primary Care of the Posterior Segment. Norwalk, Conn.: Appleton & Lange, 1994: 89-170.
|
Next Month in the Mag |
|
6th Annual Dry Eye Report: Dry Eye is a Disease! Feedback |

