Today’s optometrists are increasing their utilization of non-invasive technologies to aid in the observation of retinal tissues.
OCT may have already supplanted the ‘gold standard’ fluorescein angiography for detecting some retinal etiologies, such as cystoid macular edema.
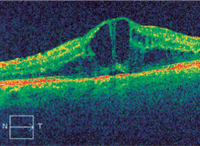
Ocular coherence tomography (OCT) facilitates evaluation, monitoring and follow-up for glaucoma and macular pathologies. In addition, OCT can be beneficial in numerous retinal manifestations to establish tissue thickening or thinning when compared to the normal population database.
While fluorescein angiography has been the “gold standard” of evaluation and management of macular and retinal pathologies, OCT has augmented or even replaced angiography in particular cases. Cystoid macular edema, central serous retinopathy and diabetic maculopathy are only a few of the macular pathologies where OCT proves to be extremely beneficial.1
Since the introduction of the OCT, optometrists have rewritten our optometric algorithms in the diagnosis, management and follow-up of patients. This technology has allowed for increased efficacy of referrals and continued in-office management of patients. In this regard, the wider use of OCT may have a beneficial impact for the patient, as well as the doctor.
This article examines the OCT’s revolutionary technology, addressing benefits from a clinical view, in addition to an investment standpoint. It also discusses professional opinions, clinical diagnoses, management and follow-up modalities that suggest the OCT is not only important in primary care optometry, but becoming a valuable adjunctive asset for optimal patient care.
Clinical Uses for OCT
OCT affords us a highly quantifiable, accurate and repeatable technology that is best utilized in conjunction with other available subjective and objective technologies. We can utilize OCT for many types of posterior polar evaluations, such as optic nerve abnormalities, glaucoma progression, macular and retinal pathologies.
Resolution of this technology in the last several years has gone from approximately 10µm microns to 4µm. This instrument is essentially able to measure within the accuracy of two-thirds the width of one red blood cell. (Practically speaking, we are able to examine living tissue that is 0.25mm thick, containing 10 layers of highly specialized, nearly transparent cells. It shows us a living histology slide of the sensory retina and retinal pigment epithelium.)
Scanned information is then compared to “normal population” data in a way that is repeatable and highly accurate, with a high degree of sensitivity and specificity. Scanning devices allow us to pinpoint the exact layer damaged in glaucoma, optic nerve and macular processes.
Let’s look at each of these applications individually:
• Glaucoma. There is no question that nerve fiber loss and structural damage appear much earlier in the disease process than functional subjective visual field defects.2 OCT technology facilitates our ability to more accurately confirm or dismiss a diagnosis of glaucoma at an earlier stage of development. This fact promotes earlier intervention long before 40% of the nerve fiber loss manifests (which is necessary for subjective visual field depressions to be recorded).2 When combining scanning technologies with other clinical data, interventional therapy may be initiated much earlier when including OCT findings with visual fields.
However, OCT is not a stand-alone test for glaucoma evaluation and management. It should be viewed as a critical piece of information in the decision-making process. A good example is when the retinal nerve fiber layer (RNFL) shows superior and/or inferior thinning that is suspicious for glaucoma while the visual fields remain normal. OCT allows an added point of reference in following a patient from normal to glaucoma suspect, and finally to glaucoma patient.

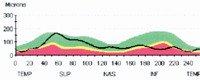
This patient’s visual field (left) correlates with his OCT TSNIT graph, which corroborates the findings of nerve fiber thinning.
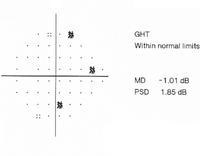
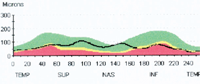
However, this patient’s visual field (left) does not agree with her OCT TSNIT graph, which suggests early nerve fiber thinning not yet apparent with perimetry.
The valuable OCT data should be clinically confirmed by the examination findings, including the “multifactorial glaucoma risk pie.” This analysis includes history, age, race, family history, longevity and general health information. Clinical testing to be added to the decision-making process includes important information, such as pachymetry, serial intraocular pressures, visual fields, stereophotography and finally clinical experience. In short, you would rarely start therapy based only on OCT thinning, but consideration of RNFL is a valuable contribution to the decision-making process.
Looking forward, the most powerful use of this technology in glaucoma will take place when we can “marry” OCT structural analysis with functional testing of visual field analysis. (Several companies are now working on producing this combined testing technology.)
Although this information is not diagnostic, it does provide relevant structural analysis to verify stability vs. progression.
• Optic nerve abnormalities. In addition to glaucoma, OCT can be used in contributing information in the areas of optic nerve drusen, optic pits, optic atrophy disorders and optic nerve edema.3 Another example would be in progressive thinning in the optic atrophies by serial analysis.
RNFL analysis can be helpful in assessing nerve head thickening in a patient with suspected pseudotumor cerebri (PTC). I have found it especially helpful in follow-up monitoring of disc changes once treatment has begun for PTC.4 This management, in conjunction with other ocular, physical and neurological examinations, can be helpful in assessing the patient’s treatment progress.
• Macular abnormalities. OCT analysis of the macula includes a range of disorders, such as:
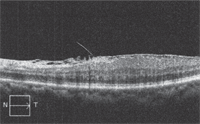
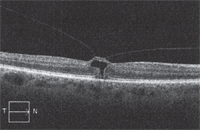
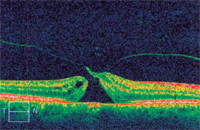
This series of OCT images, from different patients, demonstrates the development of a macular hole, starting here with epiretinal membrane with subsequent macular thickening.
An impending macular hole secondary to vitreomacular traction.
An early macular hole.
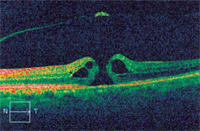
A macular hole with overlying posterior vitreous detachment.
—Macular degeneration/choroidal neovascular membrane. Scanning technology is important for initial substantiation of macular thickening when combined with clinical findings of deep and superficial retinal hemorrhages, deep and superficial exudate, fluorescein angiography, as well as subjective symptoms of metamorphopsia. OCT can show structural thickening and distortion of the macular anatomy. In addition, its usefulness has been documented to follow the success or failure of anti-VEGF therapies; it allows us serial review post-injection to structurally document the reduction of macular thickening.5 This becomes a valuable tool in guiding therapy and follow-up decisions for re-injection vs. monitoring.
—Vitreomacular traction syndromes. Scanning technology is valuable in the verification and diagnosis of these syndromes as they progress from preretinal fibrosis, classic vitreomacular traction syndrome and, finally, differentiation of early macular hole formation to complete macular hole formation. As with other disorders, this information provides structural evidence of deviation from normal macular anatomy in its various forms.
—Macular edema. OCT has become a valuable instrument in the evaluation of macular distortion, whether from diabetic, cystoid, central serous or other disorders. It also has become valuable for the retinologist, as well as the co-managing optometrist, in post-treatment patients to monitor for resolution, exacerbation or stability of macular integrity.
—Retinal arteriovenous occlusive diseases. OCT is used to monitor central retinal venous and branch occlusions as they approach the macula. In addition, arteriolar occlusive disease with secondary macular and retinal edema can be seen initially. In long-term follow-up, thinning of the affected macular and adjacent retina will be noted in many post-arterial occlusive cases. OCT is useful in initial evaluation of macular thickening as it relates to other clinical objective and subjective findings. This becomes helpful in deciding when to refer to the retinal specialist (not to mention concurrently orchestrating multidisciplinary management of underlying systemic disease). Finally, as with the macular edemas, OCT can be useful in post-treatment monitoring for improvement, stability or exacerbation of the macular anatomy.
• Anterior segment evaluation. OCT scanning devices, although not necessarily diagnostic, can be helpful in evaluating anterior segment disorders, such as narrow angles, anterior chamber or iris abnormalities when combined with additional clinical testing, such as gonioscopy, ultrasound and other clinical apparatus.
In terms of iris thickening disorders, including iris cysts and melanomas, OCT helps us to more critically differentiate between solid vs. cystic defects.
OCT for Communication
OCT is becoming an invaluable tool not only for clinical diagnosis but also for patient education, doctor-to-doctor communication and comanagement.
Consider these uses:
• Cataract surgical referrals. In special instances, OCT provides potential contributory information in patients with reduced visual acuity that is not clearly defined by other techniques. It can offer information when there is question as to degree of, for example, cataract vs. retinal effect on visual acuity. This is helpful in macular degeneration, retinal macular fibrosis or any case of suspected macular abnormality. Although mere thickness readings cannot guarantee acuity assessment, these findings can help the practitioner more accurately predict post-surgical cataract outcomes.
In addition, OCT can be useful for visualizing macular structural abnormalities that are not clearly seen through a dense cataract. This may include subtle macular edema from diabetes, small focal venous occlusive disorders, preretinal fibrosis or more subtle early macular hole formation.
Although this cannot be used as a routine test when considering cataract referral, it can be valuable information in communication with secondary or tertiary care providers in the event they are concerned that macular abnormalities may affect the visual acuity outcomes post-cataract surgery. In the same way, it can be helpful in certain refractive surgical candidates.
In short, OCT should be used in a case of “reasonable suspicion of abnormality” when we are unsure of the total visual acuity due to cataract, or a combination of cataract and macular abnormality. This technology allows the primary care practitioner a better and higher degree of competency and referral.
• Patient education. On a personal note, there isn’t a day that goes by in our office that OCT is not used in an illustrative manner. The ability to actually show the patient normal vs. abnormal tissue is highly educational. This gives the patient a better understanding of his or her disease process and/or reason we are referring for further evaluation. It also provides patients with a clear understanding of why we are monitoring their retinal tissue. This is a valuable asset in instilling patient confidence and allowing the patient to “actually see what is wrong.”
Both my patients and I have found the OCT images intuitive and easy to understand. And, patients require very little training to see how their “abnormal scan” differs from the normal.
• Teleophthalmology. The OCT provides an excellent opportunity for us to communicate with other secondary and tertiary ophthalmic physicians “over the airwaves.” This often results in a more effective referral as well as saving the patient time and money monitoring certain retinal disorders “in-house.” A simple phone call along with an e-mail of the OCT allows us a “telecommunicative consultation” to facilitate clinical decision-making between the primary and secondary care providers.
Management and Follow-up
Management of numerous posterior segment disorders with the aid of serial OCT is becoming more important in daily practice. With our present technology, follow-up of macular thickening from tractional or edematous disorders can be precisely measured to within microns. In addition to macular and retinal evaluation, no one can argue the benefit of OCT in the management and predictive value in glaucoma evaluation, both in-office and for referral to secondary glaucoma specialties.
 Comanagement is becoming a big issue in following the post-treatment macular degeneration patient who has had anti-VEGF, intraocular steroid injections, photodynamic therapeutics, or a combination of any of these. This gives the retinal specialist and the practicing optometrist the confidence in each other to comanage these patients. In particular, it gives the ophthalmologist the assurance that subtle edemas and retinal thickening, as well as other retinal fluctuations, can be more precisely monitored in the primary care office.
Comanagement is becoming a big issue in following the post-treatment macular degeneration patient who has had anti-VEGF, intraocular steroid injections, photodynamic therapeutics, or a combination of any of these. This gives the retinal specialist and the practicing optometrist the confidence in each other to comanage these patients. In particular, it gives the ophthalmologist the assurance that subtle edemas and retinal thickening, as well as other retinal fluctuations, can be more precisely monitored in the primary care office.
Because many of our retinal specialists are overworked, they welcome the opportunity to send the patient back to the referring physician’s office. The patient benefits because he is back with “the doctor I know and trust.” The cost to the health care system is arguably lower in primary vs. secondary and tertiary office settings. In addition, the patient benefits in less travel time and less wait time. Importantly, the average O.D. spends more “one-on-one” time with the patient.
Return on Investment
Even with a reduction in office reimbursements, the familiar argument that OCT is not a revenue producer is unfounded. Our office performs more than 120 OCT scans a month. True, reimbursements for OCT itself have gone down; yet, the added financial enhancement comes not only in OCT coding, but also in the charges for office visits and verification of acuities, which often requires refractions (an additional charge). This makes OCT an excellent revenue producer in the office. (See “Estimated Return on Investment.”)
Since the advent of scanning technologies in the 1980s, OCT has become more affordable and, more importantly, more valuable in patient care. The impact of this technology will make it one of the most important clinical tools available in our decade, and will only get better as technology and integration with other testing modalities improves.
The value of OCT, as with any testing technology, can only be maximized if we become familiar with the strengths and weaknesses of the equipment. Learning and experience, with a keen eye on the literature, can allow us to maximize utilization of scanning devices to enhance our ability to provide quality eye care to our community.
Dr. Bumgarner is in a primary care group practice in Pinehurst, N.C. He has no financial relationships to disclose. He thanks Andrew Apple and Nicole Piatt, fourth year optometry students at Pennsylvania College of Optometry at Salus University, for their assistance with this article.
1. Ouyang Y, Keane PA, Sadda SR, Walsh AC. Detection of cystoid macular edema with three-dimensional optical coherence tomography versus fluorescein angiography. Invest Ophthalmol Vis Sci. 2010 Oct;51(10):5213-8.
2. Quigley HA, Addicks EM, Green WR. Optic nerve damage in human glaucoma. III. Quantitative correlation of nerve fiber loss and visual field defect in glaucoma, ischemic neuropathy, papilledema, and toxic neuropathy. Arch Ophthalmol. 1982 Jan;100(1):135-46.
3. Johnson LN, Diehl ML, Hamm CW, et al. Differentiating optic disc edema from optic nerve head drusen on optical coherence tomography. Arch Ophthalmol. 2009 Jan;127(1):45-9.
4. Rebolleda G, Muñoz-Negrete FJ. Follow-up of mild papilledema in idiopathic intracranial hypertension with optical coherence tomography. Invest Ophthalmol Vis Sci. 2009 Nov;50(11):5197-200.
5. Lalwani GA, Rosenfeld PJ, Fung AE, et al. A variable-dosing regimen with intravitreal ranibizumab for neovascular age-related macular degeneration: year 2 of the PrONTO Study. Am J Ophthalmol. 2009 Jul;148(1):43-58.e1.

